 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [위 선종/이형성 (gastric adenoma/dysplasia)] - 終
[위 선종/이형성 (gastric adenoma/dysplasia)] - 終
2017년 4월 15일 순천만내시경세미나
1) 정의
2) 병리학적 진단
3) 고도/저도 등급 분류
4) 내시경 진단
5) 임상적 의의
6) 치료
9) 2014 Konkuk symposium lecture on adenoma
11) FAQ - 고도이형성은 전이 가능성이 없습니까?
12) References
 1. What is adenoma and dysplasia? 선종은 무엇이고 이형성은 무엇인가
1. What is adenoma and dysplasia? 선종은 무엇이고 이형성은 무엇인가
Doland 의학사전에서 dysplasia(이형성)는 “abnormality of development; in pathology, alteration in size, shape, and organization of adult cells”로, adenoma(선종)는 “a benign epithelial tumor in which the cells form recognizable glandular structures or in which the cells are derived from glandular epithelium”으로 정의되고 있다.
서구에서는 위 이형성 (gastric dysplasia)을 flat/depressed dysplasia와 elevated dysplasia로 나누는데 elevated dysplasia만을 adenoma로 부른다. 일본과 우리나라에서는 dysplasia를 adenoma와 거의 같은 뜻으로 여긴다. 따라서 일본과 우리나라에서는 flat/depressed adenoma와 elevated adenoma가 모두 가능하다.
서양에서는 융기형 dysplasia만 선종이라고 부르지만 우리는 융기형 dysplasia와 함몰형 dysplasia를 모두 선종이라고 부른다. 즉 우리나라와 일본에서는 "gastric dysplasia = gastric adenoma"이다.
최근 위의 암과 이형성에 대한 병리학자들의 평가가 서구와 일본에서 현저한 차이를 보인다는 점이 밝혀지고, 이를 극복하기 위한 다양한 노력이 진행되고 있다. 그러나 거의 1-2년마다 새로운 분류법이 제시되고 있으며, 그에 대한 평가가 정확하게 이루어지지 못함으로써 혼란을 부채질하고 있다. 특히 과거에는 경과관찰밖에 할 수 없었던 이형성 병소에 대한 내시경 치료가 도입되면서, 분류 및 개념통일의 필요성이 더욱 증대되고 있다.
가장 혼란스러운 것은 Revised Vienna 분류이다. 이는 대장에서는 적당할지 모르지만 위에서는 전혀 타당하지 않다. 잊어버리는 것이 낫다고 생각된다.
* 참고: EndoTODAY Opinion difference between Korea and Japan on gastric adenoma
 2. Pathologic diagnosis. 선종/이형성의 병리학적 진단
2. Pathologic diagnosis. 선종/이형성의 병리학적 진단
일반적으로 위에서의 이형성은 위상피 이형성(gastric epithelial dysplasia)을 지칭한다. 위상피 이외의 세포에서도 이형성이 발생할 수 있는데, 이와 같은 경우는 구체적으로 세포의 기원을 밝혀주는 것이 일반적이다 (예: enterochromaffin-like dysplasia).
이형성과 구분하기 어려운 개념이 선종이다. 서구에서는 위의 이형성을 편평한 이형성(flat dysplasia)과 용종형 이형성(polypoid dysplasia)으로 구분하여 용종형의 돌출된 이형성만을 선종으로 국한하여 부르기도 한다. 그러나 일반적으로는 위의 이형성과 선종을 혼용하여 사용하고 있고, 경우에 따라서는 adenoma/dysplasia와 같이 함께 기술함으로써 혼선을 피하고자 시도되기도 한다.
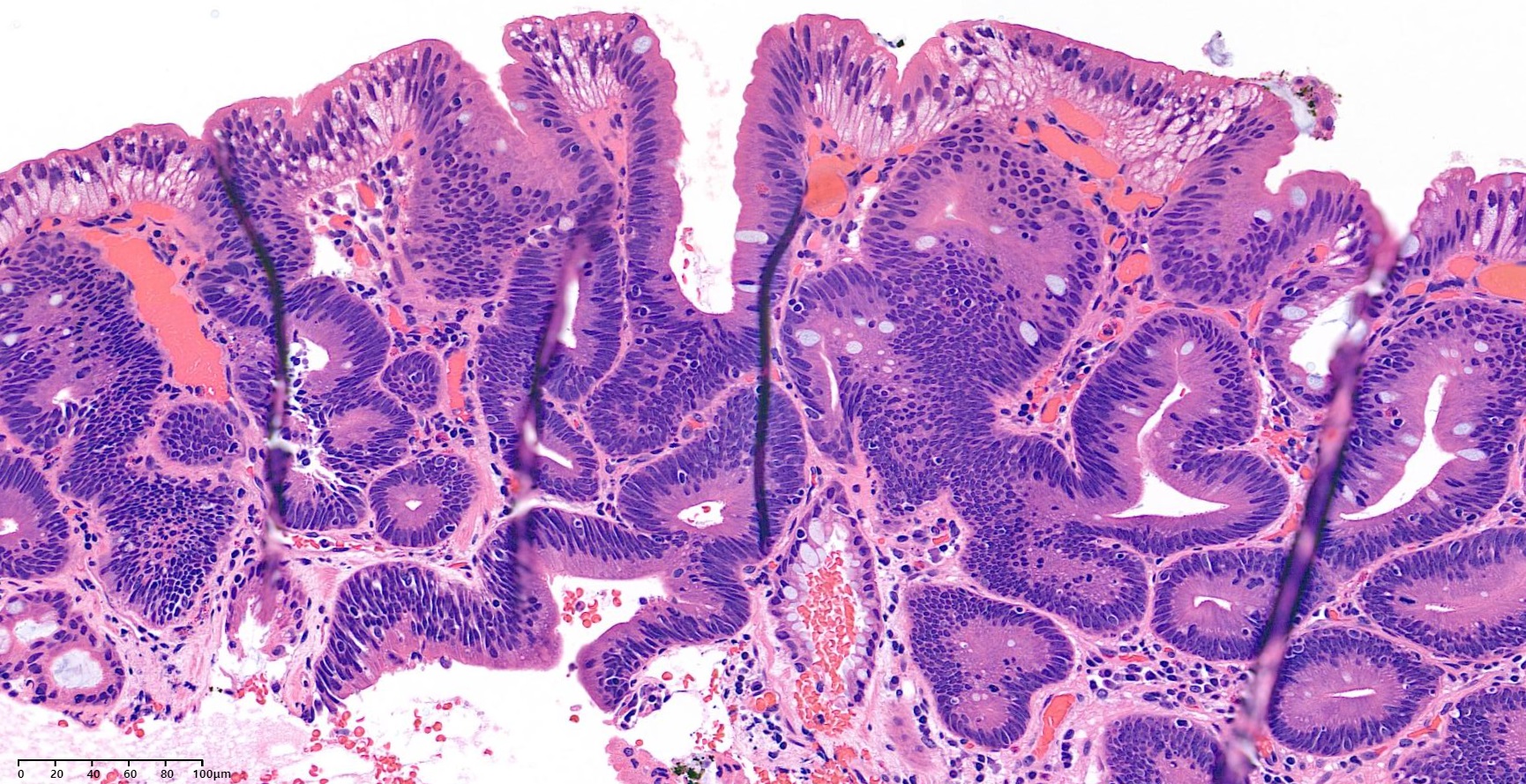
이형성의 병리학적인 특징은 아래와 같다.
| Microscopic characteristics of gastric epithelial dysplasia |
| 1) Cellular atypia
- nuclear pleomorphism - hyperchromasia - nuclear stratification - increased N/P ratio - sometimes increased cytoplasmic basophilia - loss of cellular and nuclear polarity |
| 2) Abnormal differentiation
- lack or reduced numbers of goblet cells and Paneth cells in the metaplastic intestinal epithelium - reduction, alteration or disappearance of secretory products from the gastric epithelium |
| 3) Disorganized mucosal architecture
- irregularity of crypt structure - back-to-back gland formation - budding and branching of crypts - intraluminal and surface papillary growth |
조직학적으로 이형성과 비슷한 것이 regenerating atypia인데, 이는 위점막 손상에 대한 정상적인 재생반응의 하나로 간주되는 것으로 반드시 구분되어야 한다.
세상은 analogue이다. 모든 것을 digital로 나누려는 경직성이 문제를 복잡하게 한다. 애매한 것은 애매하다고 말하는 것이 낫다.
아래는 조직검사에서 저도선종으로 나온 환자입니다. 내시경으로는 저도 선종인지 metaplastic nodule인지 거의 구분이 어렵습니다.
 3. Grading and classification. 고도/저도 등급 분류
3. Grading and classification. 고도/저도 등급 분류
병리학적으로는 다음과 같은 기준이 사용되고 있습니다.
일본에서 비정상적인 위상피 병변에 대한 최초의 조직학적인 기준은 1996년 Nakamura에 의하여 제시되었으며, 이후 1971년 Nagayo에 의하여 5개의 그룹으로 분류된 이후, 1985년 Japanese Research Society for Gastric Cancer (JRSGC)에 의하여 약간 수정되어 현재에 이르고 있다.
일본에서 사용되고 있는 5 그룹 분류의 가장 큰 문제점은 “경계성병변”으로 지칭되는 3군의 범위가 너무 넓다는 점인데, 아래에서 언급되는 Vienna 분류의 category 2와 3 및 4에 걸치는 광범위한 영역의 병변이 3군에 포함될 수 있다.
이러한 한계점에도 불구하고 5 그룹 분류는 위내시경 조직검사의 결과를 간편하게 표현하는 방식으로 이해되고 있고, 각 그룹에 따른 치료방침을 비교적 명확하게 정할 수 있으므로 일본에서는 매우 광범위하게 이용되고 있다. 또한 서양과 일본의 병리학자간의 견해를 일치시키기 위한 노력인 Vienna 분류와 Padova 분류도 기본적으로는 일본의 5 그룹 분류법에 기초하고 있기 때문에 그 영향력은 매우 크다고 생각된다.
위암의 진단에 있어서 일본과 서구의 병리학자간의 견해는 매우 차이가 크다. 일본에서는 병변의 구조와 세포학적 특징에 따라 위암을 진단하지만 서양에서는 침윤의 증거가 있을 때에만 위암으로 진단한다. 따라서 서구에서의 고도이형성의 대부분과 저도이형성의 일부가 일본에서는 위암으로 진단이 되고 있다. 또한 일본에서의 선종은 서양에서의 이형성과는 약간 다른 용어로서 내시경 혹은 육안소견과는 무관하며, 오히려 서구에서의 저도이형성에 가까운 개념이다. 따라서 일본에서는 함몰형 선종이라는 진단이 가능하다. 이에 반하여 서양에서는 일반적으로 융기형의 이형성만을 선종이라고 부르고 있다.
이와 같은 동서양의 차이에 대한 문제제기는 주로 Schlemper에 의하여 이루어졌다. Schlemper의 주도하에 1996년 동경에서 국제회의가 열렸으며, 그 결과가 1997년 “Differences in diagnostic criteria for gastric carcinoma between Japanese and western pathologists”라는 제목으로 Lancet지에 처음으로 실리면서 국제적인 주목을 받게 되었다.
이후 1998년 Vienna에서 열린 World Congress of Gastroenterology에서 consensus를 만들기 위한 회의가 열렸으며 그 결과 Vienna 분류가 제안되었고 현재까지 가장 널리 이용되고 있다. 1998년 이탈리아의 Padova에서도 consensus를 위한 회의가 열렸으며 그 결과 Padova 분류가 제안되었는데, Vienna 분류에 비하여 이용되는 빈도는 낮은 듯 하다. Padova 분류에서의 category는 JRSGC의 그룹과 거의 대등한 것으로, Padova 분류는 일본의 개념을 서양에서 거의 변형하지 않고 받아들인 것으로 이해해도 무방할 정도로 유사하다.
Vienna 분류의 제안에 참여하였던 일부 연구자들이 2000년 홍콩에서 열린 11회 Asian Pacific Congress of Gastroenterology에서 Vienna 분류를 다소 변형시킨 새로운 분류법을 제안하였다 (“revised Vienna classification”). Vienna 분류가 발표된 이후에도 서양과 일본에서 병리학적인 진단에 지속적인 차이점이 노출되었는데, 이들은 high-grade adenoma/dysplasia와 intramucosal carcinoma를 한 그룹으로 묶음으로서 동서양의 차이를 없애고자 하였다. 그러나 이형성과 암을 하나의 그룹으로 묶는다는 것은 기존의 개념으로는 받아들이기 어려운 것으로 revised Vienna classification이 널리 사용되지 못하고 있는 이유라고 생각된다.
아래는 ESD 후 저도 선종으로 판독된 증례들입니다.
아래는 16mm 고도선종입니다.
 4. Endoscopic diagnosis. 선종/이형성의 내시경 진단
4. Endoscopic diagnosis. 선종/이형성의 내시경 진단
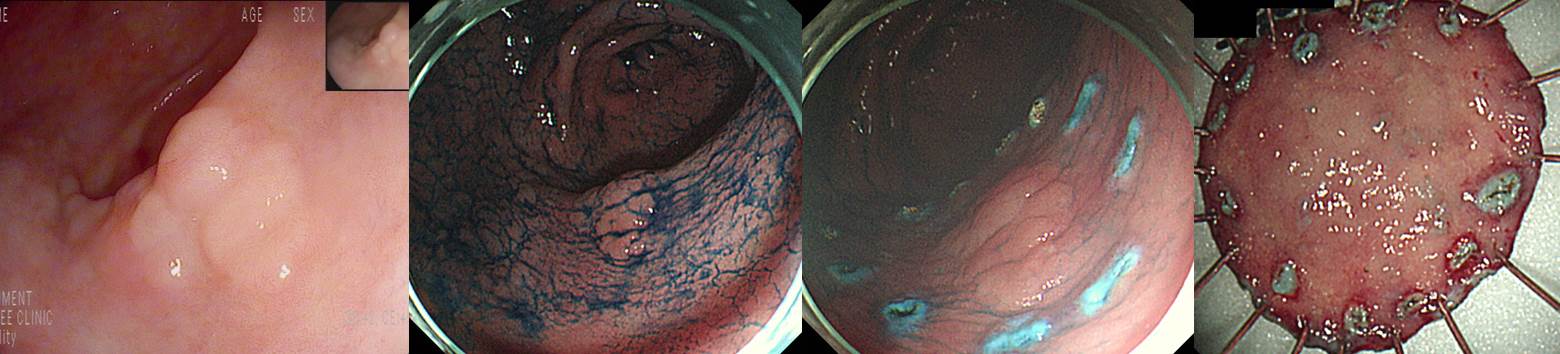
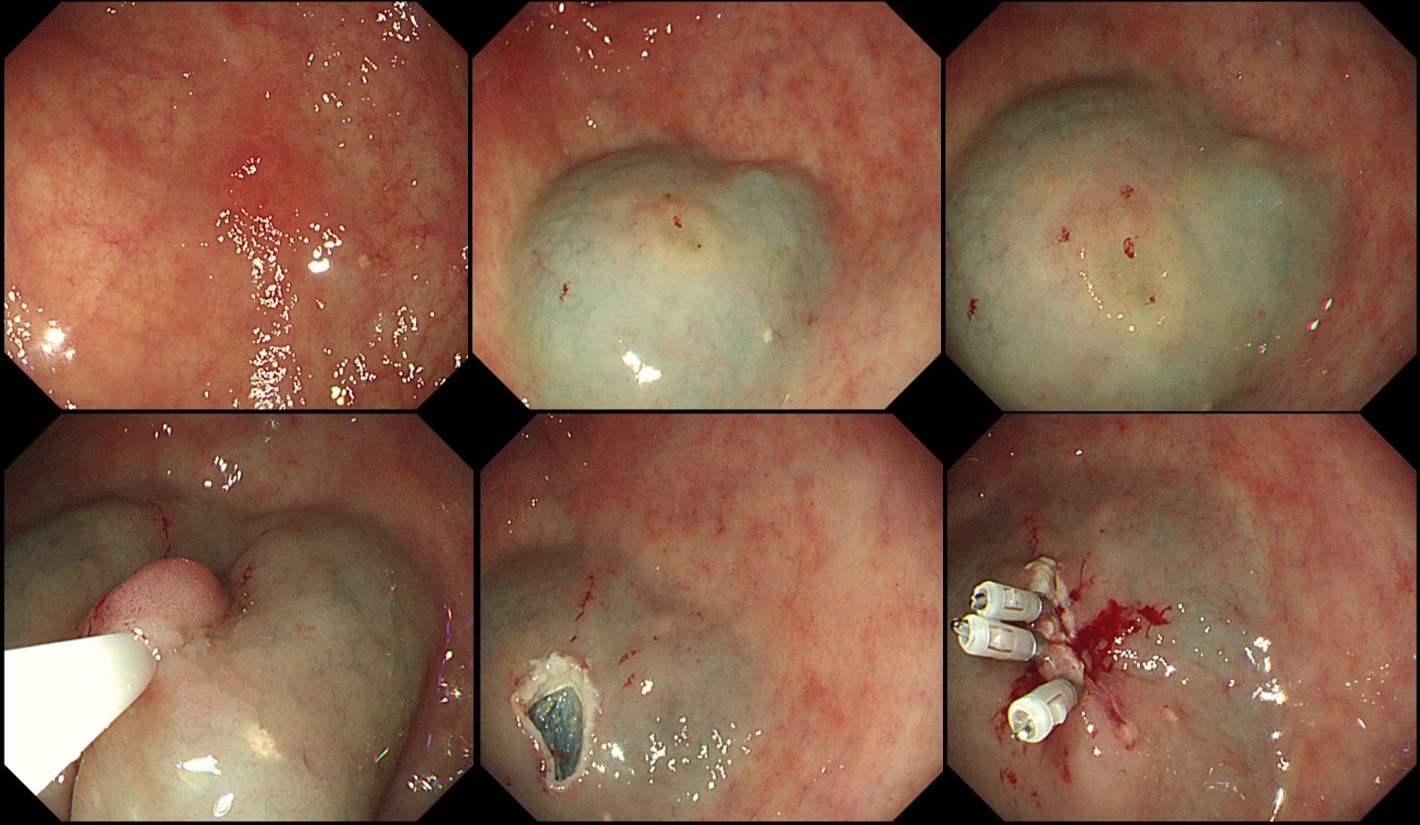
Elevated type adenoma with pseudodepression (ESD pathology: 10 mm low grade dysplasia)
Elevated type adenoma
Elevated type adenoma
80세 여성. 우연히 발견된 저도선종인데 어떠한 치료를 추천할 것인가? 경과관찰, 소작술, 절제술???
조직검사에서 adenoma with high grade dysplasia였으나 EMR 후 위암으로 진단이 바뀐 예
Depressed type adenoma. 서양에서는 adenoma라고 부르지 않는다. flat/depressed type의 병변들 서양에서는 dysplasia라고 부른다.
모양을 보고 암일 수도 있겠다 생각하였고 ESD 결과를 확인하였는데 의외로 1.4 cm 저도 선종으로 나왔음.
고도선종은 되겠다 싶었는데 저도선종으로 나왔습니다.
Stomach, endoscopic submucosal dissection:
Tubular adenoma with low grade dysplasia
1. Location : angle, lesser curvature
2. Gross type : elevated
3. Size of adenoma : (1) longest diameter, 32 mm (2) vertical diameter, 17 mm
4. Resection margin : negative resection margins(N)
타 의료기관에서 내시경 및 조직검사로 진단된 선종이나 조기위암 환자의 내시경 치료 전 내시경 재검이 필요할까요? 첫 내시경 사진을 검토하여 검사가 적절히 이루어졌고 병소에 대한 명확한 사진이 있으면 재검하지 않고 즉시 시술을 합니다. 그 과정 중 종종 추가 병변이 발견됩니다. 다행스럽게 첫 병소와 추가 병소가 매우 가까우면 한꺼번에 절제하기도 합니다. 고도선종으로 의뢰된 환자입니다. ESD를 하기 직전 추가 병소를 발견하였는데, 두 병소의 위치가 매우 가까워 한꺼번에 치료하였고 최종 병리결과도 잘 나왔습니다. "Tubular adenoma with high grade dysplasia. (1) 14 x 13 mm, (2) 10 x 8 mm, negative resection margins." 그런데 처음 사진을 자세히 살펴보니 두번째 병소가 희미하게 보였습니다 (노란 점선 화살표). 아래 증례도 거의 동일한 경우였습니다. [2017-9-10]
선종 단계를 지나 위암이 되는 부분이 전체 위암의 몇 %인지 명확하지 않습니다. 분화형 위암의 대부분이 선종 단계를 거칠 것으로 추정하고 있을 뿐입니다. 문제는 선종의 자연사가 명확하지 않다는 것입니다. 11년 전 adenoma with LGD로 진단되었고, 내시경 치료를 권했으나 환자는 추적관찰을 원하셨고, 대강 2년 간격으로 몇 번 조직검사에서 계솔 LGD로 나왔다가 11년 째 조직검사에서 HGD로 나왔습니다. ESD를 했습니다. 분명 천천히 변하는 선종이 있습니다.
LC of mid antrum, ESD: Tubular adenoma with high grade dysplasia
1. Location : antrum, lesser curvature
2. Gross type : elevated
3. Size of adenoma : (1) longest diameter, 30 mm (2) vertical diameter, 15 mm
4. Resection margin : negative resection margins(N)
84세 남성의 검진 내시경에서 발견된 병소를 ESD로 치료했습니다. 84세에서 검진이 필요한지는 의문이지만 일단 발견된 병소는 치료하지 않을 수 없는 것이 현실입니다.
ESD: Tubular adenoma with high grade dysplasia
1. Location : mid body, lesser curvature
2. Gross type : elevated
3. Size of adenoma : (1) longest diameter, 30 mm (2) vertical diameter, 27 mm
4. Resection margin : negative resection margins(N)

ESD: Tubular adenoma with high grade dysplasia
1. Location : antrum, lesser curvature
2. Gross type : elevated
3. Size of adenoma : (1) longest diameter, 25 mm (2) vertical diameter, 24 mm
4. Resection margin : negative resection margins(N)
여자 80세 저도선종입니다. 어떻게 치료하시겠습니까? 저는 소작술을 추천하였습니다.
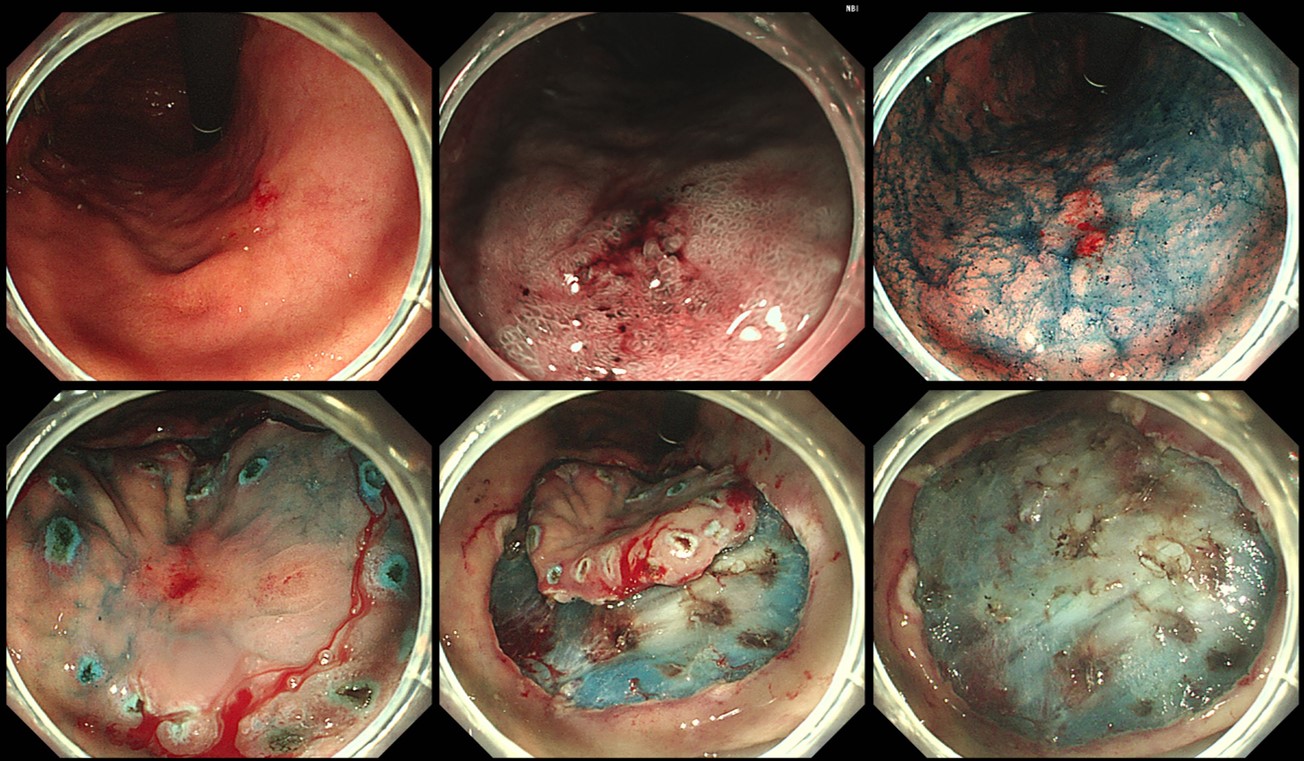
외부 조직검사에서 '중등도 이형성'이라 의뢰된 분입니다. 불규칙한 함몰형 병소이므로 위암의 가능성도 있겠다 싶었습니다. ESD를 하였는데 의외로 저도 선종으로 나왔습니다. 알다가도 모를 것이 선종입니다. (좌측 내시경 사진은 contrast가 너무 강합니다. 내시경 시스템의 enhancement를 낮춰야 합니다. Contrast가 강하면 일견 잘 보이는 것 같지만 subtle한 색조 변화는 다 놓친다고 보면 됩니다. 적당한 것이 최선입니다.)
ESD: adenoma with low grade dysplasia
1. Location : antrum, greater curvature
2. Gross type : elevated
3. Size of adenoma : (1) longest diameter, 18 mm (2) vertical diameter, 13 mm
4. Resection margin : negative resection margins(N)
 5. Clinical significance. 선종/이형성의 임상적 의의
5. Clinical significance. 선종/이형성의 임상적 의의
우리나라에서 위 dysplasia는 매우 많이 진단되고 있습니다 (2018년 18,717명, 심평원).
이형성의 예후 및 임상적 의의에 대한 조망을 위해서는 이형성의 조직학적인 진단과 분류법이 명확하여야 한다. 그러나, 앞서 언급한 바와 같이 이형성의 병리학적 분류체계가 최근까지도 계속해서 변형되고 있으므로 기존의 연구결과를 현재의 치료방침에 부합하도록 다시 해석하는 일은 매우 어려운 과제가 되고 있다.
이형성에 대한 내시경 점막절제술을 시행한 후 절제된 병변에 대한 조직학적 검사결과와 시술 전 조직검사 결과를 비교한 여러 연구의 결과들을 살펴보면 이형성에 대한 치료원칙을 세우는데 도움이 된다.
본 교실에서 내시경 점막절제술을 시행한 환자의 시술 전 조직검사 결과와 시술 후 점막절제술 병리결과를 비교해 보았을 때, 저도이형성의 1.0%에서 시술 후 위암으로 진단이 바뀌었고 고도이형성의 31.8%에서 위암으로 진단이 바뀌었다. 조직검사부터 내시경 점막절제술간의 기간이 짧기 때문에 고도이형성이 위암으로 진행하였다고 생각하기 보다는 처음부터 위암이 있었으나 조직검사 소견만으로 위암을 진단되지 못하였던 것으로 판단된다. 최근에는 이형성에 대한 조직검사의 판독 예가 증가하면서 고도이형성이 내시경 점막절제술 후 위암으로 진단이 변경되는 경우가 감소하고 있다.
궤양을 동반한 저도선종 ??? --> 결국 ESD 후 3 cm 고도선종 + 1 cm 암으로 확인되었습니다. 조직검사가 저도선종이더라도 모양이 이상하면 암을 생각해야 합니다.
[2019-11] 내시경학회에서 발표된 포스터 - Clinical outcomes of endoscopic resection for LGD and HGD on gastric pretreatment biopsy: Korea ESD Study Group
Introduction: Some cases of gastric low-grade dysplasias (LGDs) and high-grade dysplasias (HGDs) on forceps biopsy (FB) are diagnosed as gastric cancer (GC) after endoscopic resection (ER). This study aims to evaluate the clinical outcomes of ER for gastric LGD and HGD on pretreatment FB and factors predicting the pathologic upstage to GC. Patients and Methods: Patients who underwent ER for LGD and HGD on pretreatment FB from March 2005 to February 2018 in 14 hospitals in South Korea were enrolled, and medical records for the patients were reviewed retrospectively. Results: 2150 LGD and 1534 HGD diagnosed by pretreatment FB were enrolled. 589 cases of 2150 LGDs (27.4%) were diagnosed with GC after ER. Helicobacter pylori infection, smoking history, tumor location in middle third of stomach, tumor size > 10 mm, depressed lesion, and ulceration significantly predicted GC. 1129 cases of 1534 HGD (72.7%) were diagnosed with GC after ER. previous history of GC, Helicobacter pylori Infection, smoking history, tumor location in upper third of stomach, tumor size > 10 mm, depressed lesion and ulceration were significantly associated with GC. As the number of risk factors predicting GC increased in both LGD and HGD on pretreatment FB, the rate of upstage diagnosis to GC after ER increased. Conclusions; A substantial proportion of LGD and HGD on pretreatment FB were diagnosed as GC after ER. Accurate ER such as endoscopic submucosal dissection (ESD) should be recommended in cases of LGD and HGD with factors predicting pathologic upstage to GC.
[위암 505 - 선종 ESD 후 위암으로 진단이 바뀐 증례]
우연히 시행한 검진 내시경에서 전정부 대만의 선종이 발견되었습니다. 의뢰 전 조직검사 판독은 "atypical gland proliferation , favoring adenoma, low grade dysplasia"였으며 의뢰 후 외부슬라이드 재판독 결과는 "adenoma, focal high grade dysplasia"였습니다. 표현은 약간 다르지만 내용은 거의 비슷하다고 할 수 있습니다. 외부 병리 선생님의 판독을 의역하면 '저도 선종인데 gland가 약간 atypical하다 (= 저도 선종 치고는 약간 심하다)' 정도가 될 것이고, 본 병원 병리 선생님의 판독은 '고도 선종인데 focal하다 (= 고도 선종 치고는 약간 얌전하다)' 정도입니다. 두 분 모두 저도 선종과 고도 선종의 중간 아닌가 정도의 판독을 주신 것입니다.
저도 선종 ESD 후 위암으로 진단이 바뀌는 경우는 5-10%입니다. 고도 선종 ESD 후 위암으로 진단이 바뀌는 경우는 33%-50%입니다 (EndoTODAY Diagnostic group classification). 저도 선종과 고도선종의 중간 정도라면 ESD 후 암으로 진단이 바뀔 가능성도 이 중간 어디쯤일 것입니다. 대략 20% 정도?
전체적으로 6.9% (141/2,041)가 down-grade 되고 15.9% (324/2,041)가 up-grade 되었습니다. Diagnostic group classification이 그렇게 바뀌었다는 의미입니다. (Lee JH. Surg Endosc 2016)
ESD를 시행하였고 결과는 아래와 같았습니다.
Stomach, endoscopic submucosal dissection:
. Early gastric carcinoma
1. Location : antrum, greater curvature
2. Gross type : EGC type IIa
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 11 mm (2) vertical diameter, 10 mm
6. Depth of invasion : invades mucosa (lamina propria) (pT1a)
7. Resection margin : free from carcinoma(N), safety margin : distal 10 mm, proximal 10 mm, anterior 8 mm, posterior 16 mm
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent과거 4박 5일 CP(clinical pathway)로 시술할 때에는 퇴원 전 병리결과가 나왔습니다. 정부의 입원기단 단축 압력으로 인하여 CP를 3박 4일로 바꾼 후로는 퇴원 전 병리결과가 나오지 않기 때문에 외래에서 설명을 하고 있습니다. 저는 아래와 같이 설명하였습니다. 사전에 암 가능성을 충분히 알려드렸기 때문에 환자가 크게 놀라는 일은 거의 없습니다.
위 선종/이형성(adenoma/dysplasi)에 대한 치료방법 중 가장 적극적인 방법은 위절제술이지만 최근에는 거의 사용되는 예가 없으며, 대부분 내시경을 이용한 치료가 이용되고 있습니다. 위암의 경우에 내시경점막절제술은 비록 장기간의 추적관찰 성적이 부족하고 시술자마다 각기 다른 치료방법이 사용되고 있다는 한계는 있으나, 적응증을 만족하는 일부 조기위암의 근치적 치료법의 하나로 인정되고 있습니다.
특히 내시경점막하절제술(ESD: endoscopic submucosal dissection) 방법이 도입되면서, 과거보다는 훨씬 큰 병변에 대한 일괄절제가 가능해지면서 내시경치료의 적응증을 넓혀가는 추세입니다. 이형성의 경우에는 어떠한 내시경 치료법이 최선의 방법인지에 대한 통일된 의견이 없으나, 내시경 치료의 적응증이 되는 위암과 고도이형성의 생물학적인 특성이 크게 다르지 않다는 관점에서 동일한 치료법을 적용하는 것이 일반적입니다. 그러나, 이형성에 대한 내시경치료에 있어서 아직까지 해결되어야 할 많은 과제가 남아있습니다.
(1) 고도이형성에 대해서 내시경치료를 시도하는 것은 일반적으로 인정되고 있으나, 저도이형성도 적극적으로 치료를 할 것인지 혹은 위험인자를 동반한 저도이형성만을 선택적으로 치료할 것인지에 대한 논의가 지속되고 있습니다. 2014년 리뷰(건국대 이선영)에서 언급된 바 있듯이 우리나라와 일본의 병리학적 진단기준 차이에 따른 혼란이 상당합니다. 이 이슈가 제기된 것이 20년이 넘었지만 아직도 거의 좁혀지지 않은 것 같습니다. 우리나라에서는 우리나라 병리의사의 기준에 따라 치료법을 선택할 수 밖에 없다고 생각합니다.
고령 환자에서 저도 선종이고 내시경 소견이 융기형이고 pale한 경우는 조심스럽게 경과관찰을 할 수 있다고 생각합니다. 물론 소작술로 간단히 치료할 수 있기도 하지만...
(2) 소작술: 선종에 대한 표준적인 치료법의 내시경 절제술이지만 간혹 내시경 소작술도 사용되고 있습니다 (소작술  ). 그러나 치료법 선택의 기준은 여전히 불명확합니다. 소작술은 절제술에 비하여 비교적 안전하며, 입원을 하지 않고 외래에서 시행하기도 하며, 아르곤 플라즈마 응고소작술이라는 기술적인 난이도가 높지 않은 방법이므로 최근 그 이용 빈도가 증가하고 있습니다. 그러나 소작술은 치료한 병변에 대한 완전한 조직학적인 검토가 불가능하며, 특히 아르곤 응고 소작술의 경우 기존의 전기응고소작술이나 레이저소작술에 비하여 조직이 파괴되는 깊이가 얕다는 단점도 있으므로, 위험인자가 없는 저도이형성 이외의 고도이형성에 대한 소작술은 다소 위험하다고 생각합니다.
). 그러나 치료법 선택의 기준은 여전히 불명확합니다. 소작술은 절제술에 비하여 비교적 안전하며, 입원을 하지 않고 외래에서 시행하기도 하며, 아르곤 플라즈마 응고소작술이라는 기술적인 난이도가 높지 않은 방법이므로 최근 그 이용 빈도가 증가하고 있습니다. 그러나 소작술은 치료한 병변에 대한 완전한 조직학적인 검토가 불가능하며, 특히 아르곤 응고 소작술의 경우 기존의 전기응고소작술이나 레이저소작술에 비하여 조직이 파괴되는 깊이가 얕다는 단점도 있으므로, 위험인자가 없는 저도이형성 이외의 고도이형성에 대한 소작술은 다소 위험하다고 생각합니다.
저도 선종을 절제한 후 고도선종으로 바뀌는 예가 있습니다. 그러나 작고 하얗고 납작하고 궤양이 없는 저도선종이 시술 후 고도선종으로 바뀌는 예는 거의 없습니다. 작고 하얗고 납작하고 궤양이 없는 저도선종에 대하여 APC ablation을 할 수 있다고 생각합니다.
APC ablation for gastric low grade adenoma (시술 장면을 serial로 보시려면 그림을 클릭하세요.)
Flat하고 pale한 선종을 APC로 치료 후 재발 없이 경과관찰 하고 있습니다. Fujifilm으로 진단되어 의뢰되었고 Olympus로 치료하였고 Pentax로 추적관찰 하였습니다.
소작술(APC ablation)은 흔히 간단한 치료로 간주되는 경향이 있습니다. 대부분 외래 기반으로 치료가 됩니다. 그러나 드물게 출혈을 하는 경우가 있습니다. 생각보다 mucosal destruction이 크고 깊기 때문입니다. Local control은 잘 된다는 의미이기도 합니다만... 따라서 시술을 하기 전에는 늘 출혈 위험을 설명해야 합니다.
2022년 Gut and Liver 지에 아산병원에서 APC 후 출혈의 발생률을 분석한 보고가 있었습니다 (Gut Liver 2022). 출혈률은 2.4%였습니다. 항혈전제 투약 유무와 출혈률 사이에는 유의한 상관관계가 없었습니다. 적절히 끊었기 때문으로 추정됩니다.
APC 후 출혈 시점 (Gut Liver 2022)
저는 대부분 외래 기반으로 소작술을 시행하고 있습니다. 환자에서는 아래와 같이 설명을 하고 있는데 2%의 출혈률을 안내하고 있습니다. 입원치료를 권하는 병원도 있습니다.
[이준행 환자 설명서 2017의 선종 소작술 부분]
"화생성위염 - 저도선종(腺腫) - 고도선종 - 조기위암 - 진행성위암"의 단계에서 저도선종으로 나왔습니다. 선종은 다발하는 경향이 있어서 여러개가 동시에 발견되거나, 처음에는 하나였는데 나중에 몇 개의 선종이나 조기위암이 발견되는 예도 많습니다. 따라서 이번에 잘 치료하는 것도 중요하지만, 장기적이고 정기적인 검사가 꼭 필요합니다. 보통 1년에 한번 내시경 검사를 추천합니다.
선종은 과거 치료없이 경과관찰을 하다가 암이 되는 분만 개복수술을 하였습니다. 최근에는 미리 내시경치료를 합니다. 두 가지 치료법이 있습니다. 절제술은 깊게 치료할 수 있고 조직병리를 재확인할 수 있다는 장점이 있습니다. 하지만 입원이 필요하고, 합병증 위험도 높습니다. 소작술은 보통 입원이 필요하지 않고 비교적 안전하게 넓은 부위를 치료할 수 있습니다. 작고 납작한 저도선종은 주로 소작술로 치료하고 있습니다.
내시경 시술 후 1시간 정도 회복실에서 안정을 취한 후 퇴실하게 됩니다. 시술 2시간 후 (= 퇴실 1시간 후) 물이나 음료수(우유, 두유도 가능)를 마시고, 시술 3시간 후 (= 퇴실 2시간 후) 부드러운 죽을 드십시오. 다음 날 아침은 밥을 드셔도 좋습니다만 단단한 반찬은 피하십시오. 약은 2주간 하루 한 알 아침 식전에 복용하십시오. 귀가 후 출혈위험이 있습니다만, 그 빈도는 2% 정도입니다. 그 경우 연락을 주시거나 병원을 찾아주십시오. 며칠간 약간 아플 수 있습니다. 진정(수면)내시경 후 당일은 절대 운전하지 마시고, 보호자와 함께 귀가하시기 바랍니다.
위암이나 위선종이 있는 분에서 대장암이나 대장 선종도 잘 생긴다고 합니다. 따라서 아직 검사를 받지 않으셨다면 대장내시경 검사를 꼭 받아보십시요.
소작술은 대부분 저도 선종에 적용하지만 위치나 환자의 기저질환 등을 고려하여 고도 선종도 소작술로 치료하는 경우가 있습니다. 많지 않습니다.
2024년 6월 아산병원 위선종 내시경 소작술에 대한 기사가 있었습니다.
 [2025-7-21] 헬리코박터학회지에 저도 선종 치료 현황을 조사하여 발표하였습니다. (https://doi.org/10.7704/kjhugr.2025.0021) 제 생각보다 우리나라 의사들이 aggressive한 치료를 하고 계시는 모양입니다. 치료의 득과 실에 대한 면밀한 연구가 필요하다고 생각합니다.
[2025-7-21] 헬리코박터학회지에 저도 선종 치료 현황을 조사하여 발표하였습니다. (https://doi.org/10.7704/kjhugr.2025.0021) 제 생각보다 우리나라 의사들이 aggressive한 치료를 하고 계시는 모양입니다. 치료의 득과 실에 대한 면밀한 연구가 필요하다고 생각합니다.
(3) 절제술: 위선종 중 조직형이 고도 선종이고나 저도 선종이라도 크기가 큰 경우, 함몰부가 있는 경우 등에서는 절제술이 시행되고 있습니다. ESD가 가장 좋은 방법이지만 제도적인 이유로 EMR이 시행되기도 합니다. 저야 물론 ESD를 선호하고 있습니다.
Stomach: Posterior wall of low body, ESD: Tubular adenoma with low grade dysplasia
1. Location : low body, posterior wall
2. Gross type : elevated
3. Size of adenoma : (1) longest diameter, 9 mm (2) vertical diameter, 8 mm
4. Resection margin : negative resection margins(N)
고도선종은 크기와 무관하게 우선적으로 절제술을 선택하는 것이 안전합니다.
고도선종 내시경치료를 고려하는 환자에 대한 어떤 교수님의 설명서 (2018). 암으로 진단이 upgrade 될 확률, 수술이 필요하다는 결과가 나올 확률, 이소성 병소의 위험에 대한 설명이 잘 되어 있습니다.
만성신부전으로 투석 중인 환자의 KT workup 도중 발견된 고도선종에 대한 ESD.
Stomach, endoscopic submucosal dissection:
Tubular adenoma with high grade dysplasia
1. Location : prepyloric antrum, posterior wall
2. Gross type : depressed
3. Size of adenoma : (1) longest diameter, 12 mm (2) vertical diameter, 5 mm
4. Resection margin : negative resection margins(N)
위암 의심으로 조직검사를 하여 고도선종이 나왔음. EUS에서 SM invasion 의심된다고 하여 총 4번의 조직검사를 하였는데 암으로 나오지 않아 진단목적의 ESD가 권유되어 의뢰됨. 아래 사진과 같이 시술하였음. (2018년, 여자 60세)
ESD: Tubular adenoma with high grade dysplasia
1. Location : body, anterior wall-lesser curvature
2. Gross type : flat
3. Size of adenoma : (1) longest diameter, 16 mm (2) vertical diameter, 14 mm
4. Resection margin : negative resection margins(N)
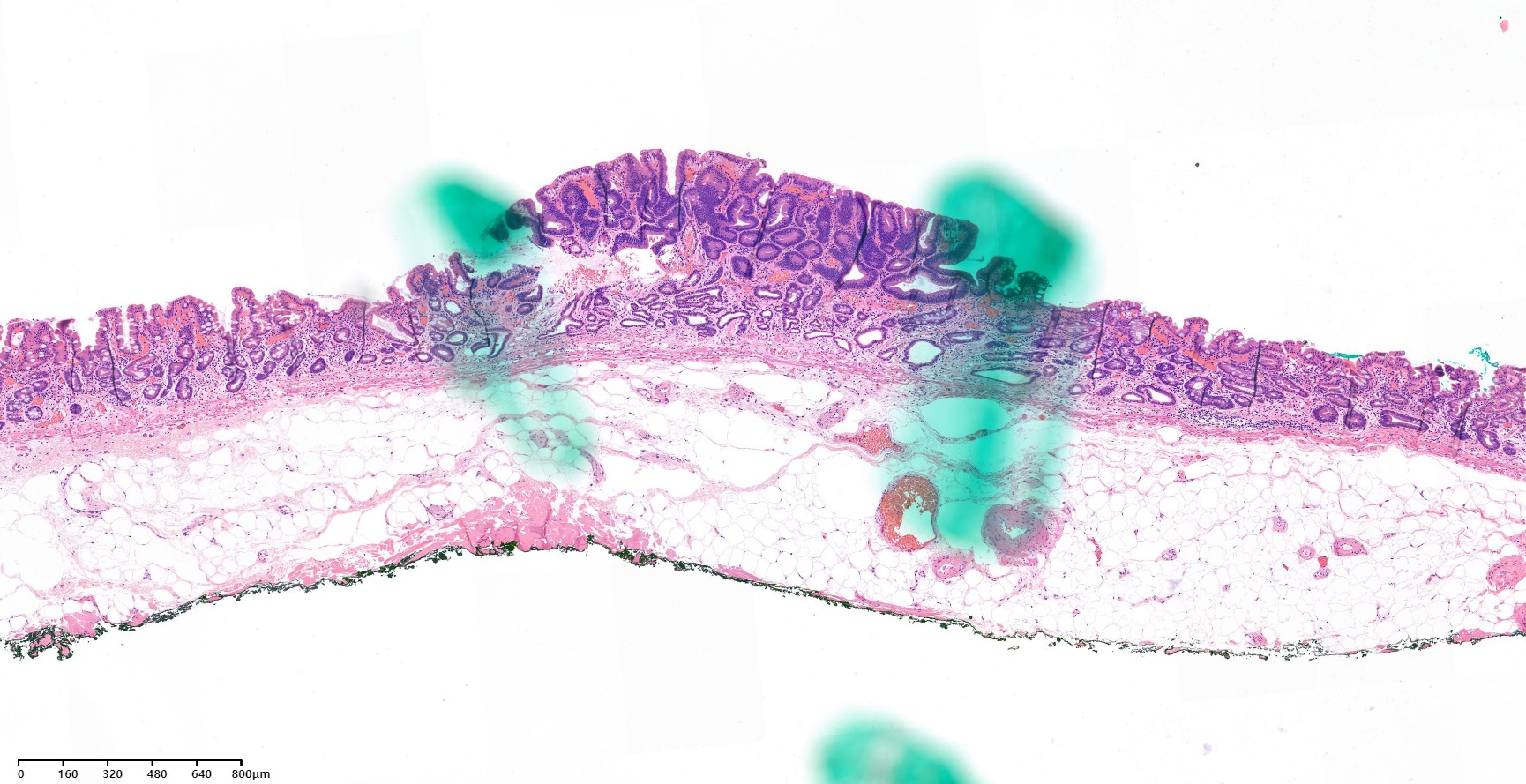
작은 융기형 병소인데 조직검사에서 high grade dysplasia로 나와 ESD를 하였고 6mm HGD로 최종 결론 (아래 병리 사진 참조)
(4) 암 치료의 일반적인 원칙에 따라 조기위암의 경우에는 다소간의 위험성이 있다고 하더라도 일괄절제를 위하여 노력하는 것은 정당화될 수 있습니다. 따라서 조기위암 환자에서는 내시경점막하절제술(ESD)과 같은 적극적인 치료를 통하여 충분한 절제연을 확보하면서 일괄절제를 할 수 있는 시술법이 널리 이용되고 있습니다. 그러나 조직학적으로 암으로 확인되지 않은 이형성 병변에 대해서도 조기위암의 치료에 사용되는 모든 방법이 동일하게 적용되어야 하는지는 명확하지 않습니다. ESD 경험이 많은 시술자는 비교적 작은 선종도 ESD로 치료하는 경향이고, ESD 초심자는 조금 큰 병소도 EMR로 치료하는 등 시술자의 경험에 따른 치료방법 선택에 차이가 있습니다. 저는 의사들이 자신의 경험과 식견을 바탕으로 최선의 치료법을 선택하도록 융통성을 인정하는 것이 좋을 것으로 생각합니다. 2018년 말 개정된 ESD 기준에서는 1.5cm 이하의 선종에 대한 ESD가 인정되지 않고 있습니다. 의사의 치료법 선택 범위를 크게 위축시키고 있는 좋지 않은 기준이므로 당장 변경되어야 합니다. 1.5cm 이하의 선종 ESD 후 조기위암으로 나온 경우는 적지 않으며, 그 중 일부는 첫 조직검사에서 저도 선종이었습니다 (아래 증례 참조). 2018년 말 개정된 기준에 따라 EMR로 치료하였더라면 다소 치료가 불충분하였을 가능성이 있습니다.
저도 선종 ESD 후 조기위암 완전절제로 나옴.
Stomach, endoscopic submucosal dissection:
Early gastric carcinoma
1. Location : proximal antrum, postero-greater curvature
2. Gross type : EGC type IIa
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 10 mm (2) vertical diameter, 8 mm
6. Depth of invasion : invades mucosa (lamina propria) (pT1a)
7. Resection margin : free from carcinoma(N) - safety margin : distal 6 mm, proximal 5 mm, anterior 8 mm, posterior 8 mm
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
(5) 국내에서는 내시경검사가 저렴하고 건강검진이 폭 넓게 시행되고 있기 때문에 건진센터 및 일차의료기관에서 내시경검사를 통하여 이형성이 진단되는 경우가 늘고 있습니다. 그러나 대부분의 이형성은 작은 융기성 혹은 함몰성 병변이므로, 첫 검사시의 자세한 정보가 전달되지 않으면 다시 시행한 내시경 검사에서 정확한 병소의 위치를 찾지 못하는 경우가 발생할 수 있습니다. 이형성의 치료를 위하여 의뢰되었으나 병소를 찾지 못한 경우에 indigocarmine과 같은 색소를 살포하면 도움이 된다는 주장도 있으나, 만성위축성 위염에 의하여 표면이 평탄하지 않은 위에서 육안적으로 자세히 관찰하여 발견되지 않았던 이형성 부위를 색소의 도움을 받아서 발견하는 것은 매우 어려운 일입니다. 따라서 이형성의 효과적인 내시경치료를 위해서는 첫 내시경 검사에서 발견된 병소의 위치, 크기, 모양을 정확히 기록하는 습관이 필요하며, 환자를 의뢰할 때에는 가급적 영상정보와 함께 자세한 자료를 함께 보내기 위한 노력이 필요합니다.
(6) 내시경 시술의와 병리의사와의 활발한 의견교환도 중요한 과제의 하나입니다. 서로의 눈높이를 맞추려는 다양한 시도에도 불구하고 아직도 서구와 일본의 병리학자들이 동일한 기준으로 위암과 이형성의 진단을 내리고 있지 못하다는 평가가 일반적입니다. 국내에서도 이와 비슷한 평가가 이루어진다면 환자의 진단과 치료에 크게 도움이 될 것으로 생각된다. 내시경 의사는 병리 소견에 대하여 어느 정도의 이해가 있어야 합니다 (EndoTODAY 위장관 병리).
 7. Cancer after ESD for adenoma with high grade dysplasia
7. Cancer after ESD for adenoma with high grade dysplasia
시술 전 조직검사: 고도선종
Stomach, ESD :
Early gastric carcinoma
1. Location : proximal antrum, lesser curvature
2. Gross type : EGC type IIa+IIc
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 52 mm (2) vertical diameter, 19 mm
6. Depth of invasion : invades mucosa (lamina propria) (pT1a)
7. Resection margin : free from carcinoma(N); safety margin : distal 9 mm, proximal 9 mm, anterior 8 mm, posterior 10 mm, deep 1800 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
위암 643
Cardia, ESD: Early gastric carcinoma
1. Location : cardia, lesser curvature
2. Gross type : EGC type IIb
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 20 mm (2) vertical diameter, 13 mm
6. Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
7. Resection margin : free from carcinoma(N), safety margin : distal 6 mm, proximal 2 mm, anterior 10 mm, posterior 12 mm, deep 900 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
고도 선종으로 ESD 후 조기위암 완전절제로 나옴.
- Histologic type : tubular adenocarcinoma, moderately differentiated
- Size : 1.6x0.7x0.05 cm
- Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
- Resection margin: free from carcinoma (safety margin: distal 1.2 cm, proximal 1 cm, anterior 1.4 cm, posterior 1.4 cm)
- Lymphatic invasion : not identified
- Venous invasion : not identified
High grade dysplasia라는 조직검사 결과로 의뢰된 환자입니다. Olympus 내시경이었습니다. 그러나 함몰형 병소의 크기와 경계를 살펴보았을 때 위암의 가능성이 높다고 판단되었습니다.
ESD를 시행하였습니다. Pentax 내시경이었습니다.
ESD: Early gastric carcinoma
1. Location : antrum, lesser curvature-posterior wall
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 20 mm (2) vertical diameter, 15 mm
6. Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
7. Resection margin : free from carcinoma(N), safety margin : distal 7 mm, proximal 9 mm, anterior 8 mm, posterior 24 mm, deep 800 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
13. Associated finding: Gastritis cystica
 8. Cancer after ESD for adenoma with low grade dysplasia
8. Cancer after ESD for adenoma with low grade dysplasia
건강검진에서 우연히 발견된 r/o EGC에 대하여 조직검사를 시행하여 adenoma with low grade dysplasia가 나왔고 1달 후 추적내시경 조직검사에서 위암으로 나와 의뢰된 환자입니다. 병소는 전정부 소만의 angle 직하부에 위치하고 있었고 ESD를 시행하여 complete resection이라는 병리 결과를 얻었습니다.
육안소견에서 위암이 의심되었고 조직검사에서 adenoma가 나온 경우에는 (1) short-term follow up을 하거나 (2) 내시경적 절제술을 시행할 수 있습니다. Short-term follow up에서 암이 나오면 진단이 끝나지만, 암이 나오지 않는 경우는 치료방침 결정이 모호해질 수 있습니다. 따라서 저는 애매한 결과가 나올 수 있는 short-term follow-up보다는 보다 확실하게 조직진단을 할 수 있는 내시경절제술을 선호하는 편입니다. 모든 선종을 ESD할 필요는 없지만 육안소견상 조기위암이 의심되는 경우에는 ESD를 시행할 수 있다고 여겨집니다.
고도 선종 ESD 후 암으로 나오는 경우는 워낙 많아서 (33-50%), 저도 선종 ESD 후 암으로 나온 경우를 중심으로 몇 증례를 소개합니다.
저도 선종 ESD 후 조기위암 완전절제로 나옴.
ESD: Early gastric carcinoma
1. Location : antrum, greater curvature
2. Gross type : EGC type IIa
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 10 mm (2) vertical diameter, 6 mm
6. Depth of invasion : invades mucosa (lamina propria) (pT1a)
7. Resection margin : free from carcinoma(N), safety margin : distal 12 mm, proximal 12 mm, anterior 14 mm, posterior 12 mm, deep 500 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
저도 선종으로 의뢰된 분입니다. 비록 외부 사진이 매우 희미했지만, 육안소견이 융기 + 함몰형으로 심상치 않다고 판단되었습니다. ESD 하였고 역시 암으로 나왔습니다.
ESD: Early gastric carcinoma
1. Location : angle
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 18 mm (2) vertical diameter, 7 mm
6. Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
7. Resection margin : free from carcinoma(N), safety margin : distal 17 mm, proximal 7 mm, anterior 10 mm, posterior 12 mm, deep 1500 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
저도 선종 ESD 후 수술이 필요한 위암으로 판정됨.
Stomach, endoscopic submucosal dissection:
Early gastric carcinoma
1. Location : low body, posterior wall
2. Gross type : EGC type IIa
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 36 mm (2) vertical diameter, 22 mm
6. Depth of invasion : invades submucosa, (depth of sm invasion :800 ㎛) (pT1b)
7. Resection margin : safety margin : distal 2 mm, proximal 5 mm, anterior 2 mm, posterior 2 mm, deep < 50 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
저도 선종 ESD 후 수술이 필요한 위암으로 판정됨 (2016)
Stomach, ESD: Early gastric carcinoma
1. Location : low body, lesser curvature
2. Gross type : EGC type IIa
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 24 mm (2) vertical diameter, 14 mm
6. Depth of invasion : invades submucosa, (depth of sm invasion : 750 ㎛) (pT1b)
7. Resection margin : free from carcinoma(N); safety margin : distal 7 mm, proximal 5 mm, anterior 12 mm, posterior 4 mm, deep 150 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
선종에 대한 conventional endoscopic resection 후 암이 나오는 경우가 제법 많습니다. 적지 않은 경우에 resection margin이 충분하지 못하여 '처음부터 ESD를 했더라면 더 좋았을텐데'라고 후회하게 됩니다. 2020년 현재 1.5cm이 안 되는 선종에서는 ESD를 할 수 없기 때문에 conventional EMR이 시행되는 경우가 많습니다. 술기상의 어려움 때문인 경우도 없지 않지만... 환자를 위한 최선의 진료를 할 수 있는 환경을 만들고 싶습니다.
선종에 대한 inject and cut 방법의 EMR 후 SM invasion이 있는 cancer이고 resection margin이 충분하지 않다고 의뢰된 환자입니다.
Outside slide reading: EMR; ADENOCARCINOMA, MODERATELY DIFFERENTIATED, arising from tubular adenoma
1. Location : body (according to outside report)
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 8 mm (2) vertical diameter, 6 mm (according to outside report)
6. Depth of invasion : invades submucosa, (depth of sm invasion : 300 ㎛) (pT1b)
7. Resection margin : free from carcinoma(N) safety margin : closest lateral, 0.2 mm (in given specimen), deep, 80-90㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
내시경 추적검사를 하였고 suspected high grade dysplasia가 나와 ESD를 할 수 밖에 없었습니다. Fibrotic scar 때문에 이런 경우의 ESD는 만만치 않습니다.
조직검사 선종이라도 조금이라도 의심스러우면 크기와 무관하게 ESD를 할 수 있게 되었으면 좋겠습니다 (2020-2-11. 이준행)
[저도 선종으로 의뢰되었으나 외부 슬라이드 재판독에서 고도선종이고 암의심된다고 나와 ESD를 하였고 점막암으로 최종 확인된 증례]
외부 슬라이드 재판독: Atypical glands, high grade dysplasia versus tubular adenocarcinoma, well differentiated. ESD is recommended.
 9. 2014 Konkuk symposium lecture on adenoma (LJH)
9. 2014 Konkuk symposium lecture on adenoma (LJH)
There are no generally accepted definitions of dysplasia and adenoma of the stomach. Dysplasia is best defined as an unequivocal neoplastic epithelial alteration. Detailed histological findings of gastric dysplasias have been described in many literatures. However, endoscopic or gross findings of gastric dysplasia need to be studied in more detail. Macroscopically, two types of dysplasias are recognized: elevated dysplasia and flat/depressed dysplasia.
Definition for adenoma is somewhat confusing. In the western countries, adenomas mean elevated or nodular lesions with dysplasia in histology, so only elevated type of dysplasias are considered as adenomas. In the eastern countries, however, both elevated and flat/depressed types of dysplasia are considered as adenomas. Actually, the terms dysplasia and adenoma are thought to be the same thing in the clinical practice. The difference is who prefers what. Usually, pathologists prefer dysplasia, and endoscopists prefer adenoma.
Dysplasias are graded as either high grade or low grade. So, adenomas (= dysplasias) can be divided as adenoma with low grade dysplasia (LGD) and adenoma with high grade dysplasia (HGD). In Korean pathologists' tradition, adenoma usually means adenoma with LGD.
In Korea, gastric adenomas with HGD are usually treated by endoscopic resection. In the final pathology for the resected specimen, 1/3 to 1/2 of adenomas with HGD are upgraded as cancer. Therapeutic approach for adenomas with HGD should be the same for early gastric cancers within absolute indications for endoscopic submucosal dissection (ESD).
Situations for gastric adenomas with LGD are quite different. After endoscopic resection of adenoma with LGD, the risk of histological upgrading is relatively small. About 10-20% of adenomas with LGD are upgraded to adenoma with HGD and 5-10% are upgraded to early gastric cancers. So, the clinical options for adenomas with LGD can be resection (EMR or ESD), ablation, and observation. In the lecture, some data regarding the advantages and disadvantages of each treatment options will be discussed.
We need to start from the definition of dysplasia. What is dysplasia? Most simply, it is an unequivocal neoplastic transformation.
There are three important histological characteristics for gastric dysplasia. They are disorganized mucosal architecture, abnormal differentiation, and cellular atypia.
Based on those three characteristics, a lot of grading schemes have been proposed. Isn’t it confusing?
Recently, dysplasias are histologically divided into two groups, low grade dysplasia and high grade dysplasia.
Endoscopically, dysplasias can be divided into elevated dysplasias and flat/depressed dysplasias.
What is the relationship between dysplasia and adenoma? Definition of adenoma is somewhat confusing. In the western countries, adenomas mean elevated or nodular lesions with dysplasia in histology, so only elevated type dysplasias are considered as adenomas. In the eastern countries, however, both elevated and flat/depressed dysplasias are considered as adenomas. Actually, the two terms dysplasia and adenoma are thought to be the same thing in the clinical practice. The difference is who prefers what. Usually, pathologists prefer dysplasia, and endoscopists prefer adenoma.
Dysplasias are graded as either high grade or low grade. So, adenomas (= dysplasias) can be divided as adenoma with low grade dysplasia (LGD) and adenoma with high grade dysplasia (HGD). In Korean pathologists' tradition, adenoma usually means adenoma with LGD.
Ideally, there should be no difference in the histological diagnosis of adenoma and cancer, because everybody is using the Vienna classification. However, it’s not so simple.
The concept of cancer may be different between countries. In Japan, structural and cytological features are important. In the western countries and in Korea, evidence of invasion is much more important. Actually, we think that most cases of HGD in the western system and Korea, as well as some LGD, become carcinoma in the Japanese system.
This is a famous study comparing the pathological diagnosis of gastric neoplasm between western countries and Japan. About half of the cases were adenomas by the western point of view. However, only 7 percent were adenomas by Japanese doctors. There is a huge difference. Korean pathologists seem to be close to western doctors in the diagnosis of gastric adenomas.
This is my understanding of this confusing situation. Three blocks are adenoma with LGD, adenoma with HGD and EGC in Korea. The next three blocks are diagnoses in Japan. So, most cases of adenoma with HGD in Korea may be EGCs in Japan.
Professor Sun Young Lee at Konkuk University discussed this dilemma in the recent editorial. Most cases of low grade dysplasias are endoscopically resected in Korea, but observation is frequently chosen in Japan. High grade dysplasias are endoscopically resected not only in Korea but also in Japan. But the diagnosis is different.
The natural history of adenoma is not clear yet. In this old study, the low grade adenomas progressed to cancer in 15% in 10 years.
Excluding palliative surgeries, we have endoscopically or surgically treated more than seventeen hundred gastric cancers in 2012 at Samsung Medical Center. Among them, 72% were early gastric cancers. In early gastric cancers, cases within absolute indications were 25%. There were 263 cases of gastric adenomas in a single year.
This is an example of endoscopically treated adenoma with low grade dysplasia.
Almost the same thing except that it was an adenoma with high grade dysplasia.
I performed ESD for a small depressed adenoma with LGD.
However, the final ESD pathology was adenocarcinoma.
It’s another example of gastric cancer with initial biopsy of adenoma. In this case, the initial biopsy was adenoma with low grade dysplasia.
In this old report from my institution, 7 out of 22 adenomas with HGD were actually carcinomas in the endoscopically resected specimen.
We reviewed the discrepancy between pre-treatment diagnostic groups and post-treatment diagnostic groups. As you can see in this complicated slide, the rate of discrepancy is more than expected. For adenoma with LGD, about 34 percents were upgraded as high grade dysplasias or cancers. For adenomas with HGD, 34 percents were upgraded as cancers.
This is a personal communication. About 1/3 to half of cases with high grade dysplasia are upgraded into cancers at Samsung Medical Center, Gangnam Severance Hospital, and Asan Medical Center.
In this report from Yonsei University, 51 out of 273 endoscopically resected low grade adenomas were upgraded into either HGD or adenocarcinoma. They evaluated the risk factors for upgrading, and recommended endoscopic resection for larger lesions and lesions without white discoloration
So, small pale flat elevated low graded adenomas can be easily treated by ablation therapy using argon plasma coagulation.
Ladies and gentlemen. I’d like to conclude my short presentation. For adenomas with HGD, endoscopic resection, preferably ESD, is recommended. For adenomas with LGD, endoscopic resection is preferred for larger lesions or lesions with central depression. Ablation is an easy and effective treatment for small pale flat/elevated adenomas with LGD.
우리나라에서 위내시경은 너무 쉽게 진행됩니다. 위암 검진 개념으로 무증상 성인에서 시행되는 경우는 물론이고, 비특이적 복부 증상을 가진 환자에서 복부 진찰이나 혈액검사보다 먼저 위내시경이 시행되기도 합니다. 그 결과 증상에 대한 평가가 충분하지 않은 상태에서 위암이나 위선종으로 상급병원으로 의뢰되는 경우가 있습니다. 저는 위선종 ESD 전 CT를 시행하는 경우가 많습니다. 주된 이유는 ESD 후 위암으로 진단이 바뀌는 예가 많기 때문입니다만, 증상에 대한 평가가 부족하였을 가능성을 고려하는 것도 또 다른 이유입니다. 이 과정에서 매우 많은 incidental finding이 발견됩니다.
아래 환자는 위선종 ESD를 위하여 의뢰되었고 시술 후 고도선종으로 확인되었습니다. 그런데 위 ESD 전 CT에서 대장암이 의심되었고, 대장내시경에서 두 개의 대장암이 발견되어 대장도 수술을 하였습니다.
[2015-5-5. 애독자 질문]
[2015-5-5. 이준행 답변]
위 저도 선종 치료법 선택에는 많은 것을 고려해야 합니다. 가장 적극적인 ESD부터, 중간 정도인 ablation, 다소 보수적인 careful observation, 가장 보수적인 무시 등 여러 전략이 가능합니다. 70대이고, 과거 위암 수술 받으신 분이고, 납작하고 흰색인 저도선종이므로 담당 선생님께서 1년 후 추적내시경을 권하신 것은 acceptable 한 선택으로 생각합니다. 물론 제 환자라면 ablation 혹은 resection을 권하였을 것 같기는 합니다. 아직 표준적인 치료법이 정립되지 않은 상태의 질환이므로 의사 사이의 치료법 선택에 차이가 있을 수 있다고 보는 것이 좋겠습니다. 70대 중후반 환자의 저도선종에서 1년 후 추적내시경이 꼭 잘못된 선택이라고 말하기는 어렵다고 생각합니다.
[2015-5-5. 환자 보호자 질문]
큰 고도선종으로 의뢰된 환자의 보호자가 고령(80대 중반)인데 내시경 치료가 필요한가 문의하여서 아래와 같이 답해 드렸습니다.
[2016-5-31. 애독자 질문]
날마다 보내주시는 엔도투데이 감사합니다. PW/antrum 병소이며 EGC가 나올 것으로 예상했는데 조직검사는 tubular adenoma 였습니다.
* Stomach, antrum, posterior wall, endoscopic biopsy ; Suggestive of tubular adenoma, focal high grade dysplasia, (see note) with
1. Erosion.
2. Focally back to back or fused pattern.
3. Combined regenerated atypia.* Microscopic findings by Sydney system ;
1. Neutrophils : absent
2. Mononuclear cells : moderate
3. Atrophy : absent
4. Intestinal metaplasia : mild
5. H.pylori : absent in Giemsa stain* Note : Endoscopic mucosal resection is recommended for excluding higher grade lesion.
조직검사에서 focal high grade dysplasia가 있었고 또 저의 내시경 소견이 EGC였기 때문에 인근 대학병원으로 의뢰했습니다. 그쪽에서 저희 조직슬라이드 review해 주신 결과와 내시경 조직검사 재검 결과는 다음과 같았습니다.
저희 슬라이드 재판독: Stomach, antrum, posterior wall, endoscopic biopsy: Tubular adenoma with low grade dysplasia.
인근 대학병원 조직검사 재검: Stomach, posterior wall of antrum, endoscopic biopsy: Tubular adenoma with low grade dysplasia (Immunoexpression of tumor: MUC5AC: weakly positive)
생각보다 조직검사 결과가 약하게 나와서 괜한 겁을 주었다고 할까봐 살짝 신경이 쓰입니다. 위암 가능성이 최소 50%라고 했거든요...
사실 local에서 special stain까지 검사할 일도 없습니다. 여기서는 H&E stain, Giemsa stain 정도를 봅니다. 조직검사 special stain은 어떤 것을 어떤 경우에 하는지, 그게 어떻게 도움이 되는지, 또 의미가 어떤 것인지 궁금할 때가 있습니다. Special stain에 대해서 내시경 학회나 연수강좌 같은데서도 딱히 다뤄준 적이 없었던 것 같습니다. 뭔가 낯설은 stain들을 만나면 그 의미를 모르다보니 답답할 때가 있습니다.
[2016-6-6. 이준행 답변]
일견 조기위암 같은데 선종으로 나온 경우입니다. 흔한 일입니다. 그 반대도 많습니다.
저는 저도 선종의 5%, 고도 선종의 33%가 내시경 절제술 후 최종 진단이 암으로 바뀐다고 설명하고 있습니다. 물론 근거는 소속 병원의 자료입니다. 10년 이상 간격을 두고 비교해 보았는데 결과는 비슷했습니다. 내시경 및 병리 검사의 결과가 안정적이라는 뜻입니다.
이풍렬 선생님께서 1994년부터 1999년까지 삼성서울병원 자료를 분석하여 2001년 발표한 논문입니다 (Park DI. Endoscopy 2001). 저도 선종의 1%, 고도 선종의 32%가 암으로 upgrade 되었습니다.
제가 2012년 삼성서울병원 자료를 분석하여 2015년 발표한 논문입니다 (Lee JH. Surg Endosc 2015). Diagnostic group classification이라는 용어를 제안하였습니다. 저도 선종의 6.2%, 고도 선종의 34.2%가 내시경 절제술 후 암으로 upgrade 되었습니다.
연세대학교 이용찬 교수님 팀에서는 치료 전 저도 선종이 치료 후 upgrade 되는 인자를 분석하였습니다 (Kim YJ. Endoscopy 2010). 저도 선종의 18.7%가 고도 선종 혹은 암으로 upgrade 되었는데, 그 위험인자는 크기와 색깔 (non-white)이었습니다.
치료 전후 병리학적 discrepancy가 있는 경우 환자에게 어떻게 설명해야 할까요? 두 전략이 있습니다. 첫번째 방법은 주관적인 판단이나 선입견을 피하여 데이타에 근거하여 설명하는 것입니다. 즉 "당신은 암일 확률이 적게는 5% 많게는 33%입니다"와 같이 설명하는 것이지요. 두번째 방법은 주관적인 판단을 그대로 전달하는 것입니다. 즉 "내시경으로 선종 전체를 절제한 후 암으로 나오는 분이 5-33%입니다만, 아무래도 환자분은 암일 가능성이 높습니다. 적어도 절반 정도는 암일 것 같습니다"라고 설명하는 방법입니다. 여러분은 어떤 방법을 선택하겠습니까?
저는 첫번째 방법을 주로 이용합니다. 의사 입장에서야 5%, 33%가 의미있는 숫자이지만, 환자에게는 어짜피 둘 중 하나이기 떄문입니다. 암이거나 암이 아니거나... 따라서 저는 일단 최대한 객관적으로 설명하면서 최종 병리결과에 따른 추가 치료 필요 여부를 정확히 따르도록 유도하고 있습니다.
암의 가능성이 높다고 말했다가 암이 아닌 것으로 나오면 "괜히 겁이나 주는 의사"로, 암의 가능성이 거의 없다고 말했다가 암으로 나오면 "암인지 아닌지도 모르는 돌팔이"로 취급될 수 있습니다. 차라리 '조금 냉정한 교수님'으로 남는 방법이 제게는 편합니다.
물론 모르지 않습니다. 1-2차 의료기관에서는 첫번째 방법이 곤란하다는 것을 잘 알고 있습니다. 환자가 어떤 반응을 보일지 알 수 없기 때문이겠지요. 너무 낮은 숫자를 말하면 방심하고 추가 검사와 치료를 받지 않는 환자도 있을 것입니다. 그렇다고 늘 너무 겁주는 방법도 좋지 않을 것 같습니다. 상황에 따라 적절히 조정하는 수 밖에 없겠습니다.
이렇게 설명한다면 어떻겠습니까? "위암 의심병소가 있었습니다. 그런데 조직검사 결과는 암 전단계인 선종으로 나왔습니다. 조직검사는 부분 검사입니다. 전체를 살펴보면 암일 수 있습니다. 따라서 내시경 절제술이 필요할 것 같습니다. 선종을 내시경으로 절제하면 5-33%에서 암으로 나옵니다. 상급 의료기관을 추천하겠습니다. 내시경 결과지, 내시경 사진, 조직검사 결과지, 조직검사 유리 슬라이드, 그리고 소견서를 챙겨드립니다. 좋은 결과 바라겠습니다."
P.S. 면역형광염색검사는 병리과 의사가 필요에 따라 추가하고 그 결과를 고려하여 최종 병리 진단을 냅니다. 대부분의 경우 임상의사가 면역형광염색검사 결과를 따로 확인할 필요는 없습니다.
[2017-4-15 순천만내시경세미나. 질문]
외부슬라이드 재판독의 중요성을 강조하셨는데요... 유리 슬라이드가 아닌 paraffin block을 요청하는 경우가 자주 있는지요.
[이준행 답변]
대부분 외부 유리 슬라이드로 끝내고 있습니다. Paraffin block은 림프종과 같은 특수한 경우에 요청하기도 합니다만 매우 드문 일입니다. Paraffin block을 이용한 추가 검사가 필요한 경우는 대부분 본 병원 내시경 재검에서 얻은 조직을 이용하고 있습니다.
[2017-4-15 순천만내시경세미나. 질문]
치료 전과 치료 후 병리진단의 차이에 대하여 잘 설명해 주셨는데요.... 교수님은 모든 선종을 ESD로 치료하고 계시는지요? 혹시 EMR-C와 같은 전통적인 방법으로 치료하는 경우는 없는지 궁금합니다.
[이준행 답변]
시술 전 조직검사에서 고도 선종이었던 경우는 적어도 1/3에서 시술 후 암으로 진단이 바뀝니다. 따라서 원칙적으로 고도 선종은 모두 ESD로 치료하고 있습니다. 저도 선종은 less invasive한 접근이 가능하다고 생각합니다. 작고, flat하고 pale한 저도 선종은 ablation으로 치료할 수 있습니다. 그 이외는 대부분 절제술을 선택하고 있습니다. 물론 ESD로 치료하는 경우가 많지만 경우에 따라서는 EMR-P, inject and cut과 같은 보다 전통적인 절제술을 사용하기도 합니다.
전체적으로 6.9% (141/2,041)가 down-grade 되고 15.9% (324/2,041)가 up-grade 되었습니다. Diagnostic group classification이 그렇게 바뀌었다는 의미입니다. (Lee JH. Surg Endosc 2016 / PDF)
[2017-4-15 순천만내시경세미나. 질문]
선종은 저도와 고도로 나뉩니다. 그런데 간혹 저도, 중등도 (intermediate grade), 고도로 나뉜 병리 결과지를 만납니다. 중등도 (intermediate grade) 선종은 어떻게 접근하는 것이 좋겠습니까?
[이준행 답변]
병리 의사들의 표준화 노력이 부족한 것은 정말 심각한 문제입니다. 중등도 (intermediate grade) 선종으로 의뢰된 경우 외부 슬라이드 재판독을 하면 대부분 저도 선종으로 나옵니다. 따라서 저는 중등도 선종은 일단 저도 선종에 준하여 접근하고 있습니다.
[2017-4-15 순천만내시경세미나. 질문]
치료 전과 치료 후 병리진단 차이의 원인에 대하여 어떻게 생각하시는지요.
[이준행 답변]
선종이나 암으로 ESD를 시행한 후 non-neoplastic pathology가 나오면 약간 난감합니다. 그러나 드문 일은 아닙니다. 2015년 아주대 논문을 보면 (Yang MJ. Endoscopy. 2015) 저도 선종의 경우 6%, 고도 선종이나 위암의 경우 3%에서 ESD 후 non-neoplastic pathology가 나오고 있습니다.
Biopsy LGD HGD or cancer No neoplasia at ESD 39 (5.5%) 13 (2.7%) Neoplasia at ESD 664 470 이러한 원인은 크게 세 가지로 생각하고 있습니다. (1) 작은 종양은 조직검사로 제거되는 경우가 있습니다. (2) 절제술 후 표본을 2 mm 간격으로 잘라 병리 specimen을 만들기 때문에 2 mm 이하의 종양은 병리학적으로 발견하지 못할 수 있습니다. (3) 내시경 절제 당시 mislocalization도 가능합니다.
Forcep으로 작은 조직을 얻은 며칠 후 내시경을 해 보면 의외로 큰 궤양이 만들어진 경우가 있습니다. 조직검사로 상당히 큰 병소가 제거되는 수 있겠다는 생각입니다. Mislocalization (전문 용어로 '헛발질'이라고 합니다^^)은 매우 드문 것 같습니다.
* 참고: EndoTODAY Nonneoplastic pathology after ESD
[2019-8-7. 이준행 혼잣말] 조기 은퇴를 고민합니다. 너무 힘들어서.
70 years old lady visited my clinic due to an adenoma of the cardia involving at least 3/4 of the circumference, which was detected during the screening endoscopy. In the local hospital, endoscopic resction was tried but failed. Actually the procedure stopped in the middle of the marking step. Surgical treatment was recommended in that hospital. What's your option for this woman?
I decided to try endoscopic resection again, although the procedure would be very difficult. I gave full information about the advantages and disadvantages of the endoscopic treatment in this challenging situation.
Endoscopic resection (multiple piecemeal) followed by APC ablation was done. The procedure time was 42 minutes. PPI with oral steroid (4 weeks course) was given for the prevention of the stricture.
The final pathology was acceptable.
Tubulovillous adenoma with high grade dysplasia ;
1. Location : cardia
2. Gross type : elevated
3. Size of adenoma : (1) longest diameter, 24 mm (2) vertical diameter, 15 mm
4. Resection margin : involved distal resection margin by adenoma negative other resection marginsEndoscopic resection of the gastric neoplasms is getting more and more difficult for me, because easy cases are treated in the local clinic. Challenging cases are referred so often. It is time to think about early retirement.
[2019-9-3. 이준행 혼잣말]
Tubular adenoma를 대롱샘종이라고 부르나보다.
[2020-5-30. 애독자 질문] 고도이형성high grade dysplasia은 전이 가능성이 없습니까?
교수님. High grade dysplasia 는 고이형성 즉 세포가 꽤 변형된 종양이라 볼수 있다고 알고 있습니다만 임상에서는 전이가능성이 없다고 본다. 이게 맞는 건가요?
[2020-5-31. 이준행 답변]
예. 원칙상 맞습니다. High grade dysplasia는 아직 intraepithelial lesion이고 epithelial cell의 basement membrane을 침범하지 않은 좁은 의미의 non-invasive pathology입니다. 전이 가능성이 없다고 보는 것이 맞습니다. 그러나 몇 가지 tricky한 면이 있습니다.
1) 병리의사의 inter-observer variation입니다. 어떤 병리의사는 조금만 이상하면 암으로 진단하고, 또 다른 병리의사는 여간해서는 암으로 부르지 않습니다. Inter-continental difference는 잘 알려져 있고, inter-national difference도 꽤 명백하지만, 한 나라 안에서의 혹은 한 병원 안에서의 inter-oberserver variation은 어느 정도 심한지 여전히 불명확합니다. 결국 나의 조직검사 sample을 누가 판독하고 있는지, 그분의 성향은 어떤지 파악하고 있어야 합니다. 궁금하면 전화로 상의할 수 있을 수준의 communication이 가능해야 합니다. 대형 병원에서 근무하고 있는 입장에서 말씀드리면, 제가 시행한 조직검사를 여러 병리의사가 판독하고 있습니다. 내시경 소견과 병리 소견이 일치하지 않을 때에는 우선 누가 판독하셨는지를 확인하고 있습니다.
2) 조직검사 결과와 ESD 결과는 상당히 다릅니다. 조직검사는 부분 검사이고 진단 과정이므로 병리의사 입장에서는 '암'으로 부르기 어려운 상황이 많습니다. 암 같기는 한데 암이라고 단언하기 어려운 상황 말입니다. 그런 경우 고도 이형성으로 보고되기도 합니다. ESD 검체에서는 암 진단이 쉽습니다. 전체 검사이고 일차 치료를 마친 상태이므로 병리의사 입장에서는 '암'이라는 진단을 붙이는데 심리적 어려움이 덜할 것입니다.
저는 이 이슈(ESD 전후 병리 결과의 차이)를 Diagnostic Group Classification이라는 개념으로 정리하고 있습니다 (Lee JH. Surg Endosc 2016).
Results: The study patients belonged to the following pretreatment diagnostic groups; LGDs in 162, HGDs in 164, AI-EGCs in 396, BAI-EGCs in 824, and AGCs in 495 cases. Posttreatment diagnostic groups were LGDs in 140, HGDs in 121, AI-EGCs in 322, BAI-EGCs in 947, AGCs in 505, and no residual tumor in 6 cases. In general, 6.9% (141/2,041) of cases were down-graded, and 15.9% (324/2,041) were up-graded. Thirty-four percent of pretreatment HGDs (56/164) were changed to cancers after endoscopic resection. Thirty-three percent of pretreatment AI-EGCs (131/396) were re-grouped as posttreatment BAI-EGCs.The additional surgery rate in each pretreatment group was 0.6% in LGD, 4.3% in HGD, 15.7% in AI-EGC, 23.6% in BAI-EGC among the patients with initial endoscopic resection (p < 0.01).
전체적으로 6.9% (141/2,041)가 down-grade 되고 15.9% (324/2,041)가 up-grade 되었습니다. Diagnostic group classification이 그렇게 바뀌었다는 의미입니다.
결국 내시경 조직검사에서 고도이형성으로 나왔다는 것으로는 전혀 안심할 수 없습니다. 최소한 ESD 병리에서 암이 아닌 것을 확인한 후 전이 가능성이 없다고 말해야 할 것 같습니다.
3) 병원간 차이도 크고 개인간 차이도 무시할 수 없는 수준입니다. 2014년 건국대학교 심포지엄 선종 강의를 준비하면서 저희 병원과 주변 병원의 시술 전후 병리 upgrade(ESD 전 고도선종, ESD 후 암)의 비율을 간단히 알아본 바 있습니다. 제 소속 병원은 1/3 수준이었고 1/2을 조금 넘는 기관도 있었습니다. 전국적으로는 약 60% 전후인 것으로 알고 있습니다. 이 또한 자기 병리 의사의 성향을 잘 알아야 한다는 것을 보여주는 자료입니다.
This is a personal communication. About 1/3 to half of cases with high grade dysplasia are upgraded into cancers at Samsung Medical Center, Gangnam Severance Hospital, and Asan Medical Center.
4) 마지막으로 매우 가슴아팠던 증례를 소개합니다. ESD 후 extragastric recurrence의 비율은 매우 낮습니다. 그러나 0%는 아닙니다. 매우 많은 환자를 치료하다보면 소수의 안타까운 증례들을 만나게 됩니다. 아래 환자가 그런 경우입니다.
조직검사에서 고도이형성으로 의뢰되었고, ESD을 하였고, 38mm의 lamina propria 암으로 나왔고, 크기 이외의 다른 risk factor는 없었고, 정기적으로 추적검사를 하였음에도 불구하고 ESD 후 multiple hepatic metastasis가 발생하였습니다. 9개월 전 내시경과 CT는 정상이었는데도 말입니다.
ESD 5년 후 multiple metastasis. Initial ESD pathology: M/D adenocarcinoma, 38x22mm, lamina propria, RM (-), L/V (-/-)
5) 고도이형성은 전이하지 않는 병입니다. 개념상 그렇다는 말입니다. 그러나 여러 조건이 필요합니다. ESD 후 고도이형성으로 확인된 환자에 대해서는 내시경 추적검사는 하지만 CT 추적검사는 하지 않고 있습니다 (물론 고도이형성 환자에서 CT 추적검사를 하는 병원도 있습니다). 병리학적 under-estimation 된 경우를 고려하여 고도이형성 환자에 대해서 CT도 시행하여야 한다는 주장을 잘 알고 있으나 CT를 한다고 모든 상황이 안전해지는 것도 아닙니다. CT는 본질적으로 치료할 수 없는 재발을 발견하는 검사 아닙니까... CT에서 뭐가 나오면 대부분 이미 안 좋은 상황입니다. (Regional node only로 나오는 더욱 드문 경우 제외)
요약합니다. 내시경 조직검사에서 고도이형성으로 나온 경우는 대략 절반 정도 암입니다. ESD 후 고도이형성으로 결론된 경우는 전이하지 않습니다. 아주 약간의 예외는 있을 수 있습니다. 의학에서 예외가 없는 경우는 없습니다.
[2020-7-10] 위 ESD 후 adenoma with HGD로 나온 환자가 외래에서 D37 코드를 줄 수 있는가 문의하여 D13.1로 하고 있다고 설명드렸습니다. 코드는 답이 없습니다. 관공서마다 다르고 병원마다 다릅니다. 나는 내 style을 일관성 있게 유지하는 것이 답입니다. 환자에 잘해드린다고 코드를 변경하거나 평소 안 쓰던 코드를 쓰면 환자에게 해가 되는 경우가 대부분입니다. 환자에게 해가 되지 않더라도 의사 본인에게 해가 됩니다. 그냥 초지일관 합시다.
* 참고: EndoTODAY 코드
[2021-12-4. 애독자 질문] low-grade(moderate) dysplasia
교수님 안녕하십니까? 로칼에서 내시경하는 의사입니다. 대장 용종절제술을 했을때, Tubular adenoma with low-grade(moderate) dysplasia 라고 나오는 경우가 가끔 있습니다. 이렇게 나오면 좀 신경이 쓰입니다. ?
Low-grade(moderate) dysplasia 는 low grade dysplasia 와 달리 어떤 임상적인 의미 및 예후 차이가 있는 소견인지 궁금합니다. 병리선생님께 문의드리니, 옛날에는 3단계 분류법이었다가 2단계 분류법으로 변경되었다고 말씀하시고, 3단계일때의 moderate 가 2단계에서는 mild 가 되었다고 말씀하셨습니다. 3단계 분류법의 moderate 가 2단계 분류법에서는 mild가 된것은 임상적 의의 및 예후가 mild와 비슷하기 때문에 크게 신경쓸 필요가 없기 때문에 그렇게 변경된것으로 해석해도 되는지요?
용종절제후 low-grade(moderate) dysplasia 라고 나오면, 신경이 많이 쓰입니다. 완전절제되었을지 걱정도 되고요. 혹시 병리 선생님의 성향에 따라서 low-grade(moderate) dysplasia 라고 결과 내지 않고, 별의미 없다고보고 그냥 low-grade dysplasia 로 내는 병리선생님도 있지 않을까 생각도 듭니다. ?
그냥 병리적으로 좀 차이 있지만, 임상적 의미, 예후는 그냥 low grade 와 별 차이 없다고 봐도 되는지요? 아니면 high grade되기 직전 단계이니 주의해야 된다 이렇게 생각해야 할른지요? ?
관련 정보를 알 수 없어서 바쁘신 교수님께 문의드리게 되었습니다. 평소 엔도투데이로 많은 가르침을 주셔서 배울수 있는 기회를 주셔서 항상 감사드립니다.
[2021-12-4. 이준행 답변]
EndoTODAY 위선종에서 고도/저도 등급 분류에 대하여 논한 바 있습니다만 이상적인 안은 없다고 생각합니다. 근본적으로 interobserver variation이 상당한 상황에서 2단계로 나누던 3단계로 나누던 나름의 문제가 있으므로 그나마 관찰자간 차이가 적은 2단계 등급 구분법이 채택된 것으로 이해하고 있습니다.
현상은 analogue인데 해석은 digital이니 애매한 경우가 없을 수 없으며 그 결과 low-grade(moderate) dysplasia라는 모호한 결과지가 나온다고 생각됩니다. 복잡하게 생각하여 환자 개인별로 최적화된 설명을 하더라도 그다지 정확하지 않은 것은 마찬가지이므로 최대한 단순하게 접근하는 것이 어떻겠습니까? 저는 그냥 low grade dysplasia에 준하여 설명할 것 같습니다.
요약하면, low-grade(moderate) dysplasia = low grade dysplasia로 보는 것이 좋겠습니다. Keep it simple!
[2022-4-18. YouTube 질문]
안녕하세요 교수님 다름이 아니라 여쭤보고 싶은 게 있습니다. 보통 위에서 발생되는 dysplasia 는 핵 크기와 모양이 다양한 pleomorphism을 많이 띄고 있나요? Low grade 와 high grade 를 구분하는 척도가 세포, 핵의 다형성으로 구분하는거라고 배웠었는데 맞는건지 모르겠습니다.
[2022-4-19. 이준행 답변]
Dysplasia의 등급 구분 기준은 다양하고 약간 주관적일 수 있습니다. 저는 아래와 같은 자료를 참고하고 있습니다. 병리과 의사가 아닌 입장에서 가장 중요하게 생각하는 것은 nuclear stratification입니다. 비전문가의 입장에서 핵의 크기가 상피세포의 절반 이하이면 저도, 절반 이상이면 고도로 생각하고 있습니다.
[2025-5-30. 애독자 질문] Oxyntic gland adenoma
Oxyntic gland neoplasm에 대한 질문입니다. 궁금한 것은 공부중에 fundic gland polyp이 결국 oxyntic mucosa에서 발생하는 것인데 fundic gland dysplasia도 oxyntic gland neoplasm으로 볼 수는 없는 것인지 이해가 잘 가지가 않습니다. Oxyntic gland neoplasm이라 하면 Oxyntic gland adenoma 와 ADC of fundic gland type만 논하고 fundic gland dysplasia 같은 경우 찾아보면 FAP 환자에서 주의해야할 사항이라고만 논하고 있어서 개념 자체가 헷갈립니다. 엔도투데이와 위질환 내시경 아틀라스에서도 Oxyntic gland adenoma 사례로 fundic gland dysplasia를 소개해주셨는데, 혹시 FAP 환자가 아닌 경우 fundic gland dysplasia라고 병리 판독이 나온다면 oxyntic gland neoplasm으로 볼 수 있는 것일까요? 기초적인 질문 죄송합니다.
[2025-5-30. 이준행 답변]
좋은 질문 감사합니다. 저도 아직 정확히 개념과 용어를 정리하지 못했습니다. 일단 리뷰의 그림과 WHO blue book (5판)의 tumors of the stomach의 목차를 잘 보시기 바랍니다.
Gastric gland는 pyloric gland와 fundic gland (= oxyntic gland)로 나누어집니다. 이 두 종류 gland 모두 pit (= foveola)와 proper gland로 구성됩니다. Neoplasm은 pit (= foveolar epithelium)와 proper gland 모두에서 발생할 수 있습니다. 저는 아래와 같은 개념을 가지고 있습니다.
Pit Proper gland 위치 Antrum Body/Fundus Antrum Body/Fundus Non-dysplastic polyp Hyperplastic polyp ? Fundic gland polyp Dysplasia Intestinal type adenoma (=tubular adenoma) and foveolar type adenoma Pyloric gland adenoma Oxyntic gland adenoma Cancer Gastric adenocarcinoma Gastric type adenocarcinoma Adenocarcinoma of fundic gland type Pit (= foveolar epithelium)에서 발생하는 것들은 antrum이나 body/fundus의 차이가 없으므로 쉽습니다. WHO blue book 5판 92쪽 gastric adenocarcinoma of fundic gland type 설명을 보면 "This type is assumed to develop from oxyntic gland adenoma."라고 분명히 씌여 있습니다. 제가 보기에는 oxyntic gland와 fundic gland가 거의 같은 의미이며 단순히 처음 이름지은 관례에 따라 (1) non-dysplastic 병소는 fundic gland polyp으로, (2) non-cancer dysplasia 병소는 oxyntic gland adenoma로, (3) cancer는 gastric adenocarcinoma of fundic gland type로 부르고 있을 뿐인 것 같습니다. 따라서 제 멋대로 새로 이름을 짓는다면 fundic gland proper에서 발생하는 여러 질환을 (1) fundic gland polyp = oxyntic gland polyp, (2) fundic gland adenoma = oxyntic gland adenoma, (3) adenocarcinoma of fundic gland type = fundic gland adenocarcinoma = oxyntic gland adenocarcinoma로 명명하고 싶습니다. 비슷한 방식으로 pyloric gland proper에서 발생하는 것은 (1) pyloric gland adenoma = gastric gland adenoma, (2) gastric type adenocarcinoma = pyloric adenocarcinoma로 명명하고 싶습니다.
아래는 저의 주장입니다. 이렇게 간단히 정리하면 얼마나 좋을까요?
Proper gland에서 발생하는 병소에 대한 명명법 통일안 (이준행 제안. 2025-5-30) 위치 Antrum Body/Fundus Non-dysplastic polyp ? Fundic gland polyp Dysplasia Pyloric gland adenoma Fundic gland adenoma Cancer Pyloric gland adenocarcinoma Fundic gland adenocarcinoma 아직 fundic gland polyp에 대응하여 antrum의 pyloric gland proper에서 발생하는 polyp에 대한 특별한 이름은 없는 것 같습니다. 그래서 ?표 입니다.
Dysplasia와 adenoma에 대한 개념은 또 다른 문제인데, 저는 간단히 dysplasia가 있으면 adenoma로 부른다고 생각합니다. 이에 대해서는 EndoTODAY 위선종에서 자세히 기술해 두었습니다.
변명 한 마디 덧붙입니다. 저도 아직 정확히 개념과 용어를 정리하지 못한 이유는 결국 병리학자들이 각자 적당하다고 생각하는용어를 만들어 사용하였는데 이를 모아 정리하는 작업을 하지 못한 탓이 큰 것 같습니다. 특히 stomach 부분은 일본 병리의사와 서양 병리의사들이 영 의견을 맞추지 못하고 있어서 더욱 헷갈립니다. 그러나 최근 WHO blue book을 보면 과거보다는 많이 정리가 되어 있습니다. 언젠가는 통일안이 나오겠지요. 기대해 봅니다.
1) 위이형성의 진단과 치료 (text, PDF)
2) [Lecture note] Gastric adenoma: to resect, ablate, or not (2014-7-12. 2014 International Hub in Advanced Endoscopy at Konkuk University)
3) Lee SY. Gastric adenoma with low-grade dysplasia: two countries, two outcomes. Dig Dis Sci 2014 (PDF 0.2 M)
4) Shin-Fan Kuan. Pathology of gastric neoplasms (Available in the Internet, PDF 2.0 M)
5) A representative case of ESD (biopsy: adenoma, ESD: EGC) (in Korean)
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.