 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [Histological heterogeneity. Mixed. 미분화 혼재암] - 終
[Histological heterogeneity. Mixed. 미분화 혼재암] - 終
1. Histological heterogeneity의 정의
3. Management after ESD (2020년 4월 13일 현재)
4. 증례 기반 심층 토의
5. FAQ
6. References
 1. Histological heterogeneity의 정의
1. Histological heterogeneity의 정의
2015년 삼성서울병원 논문(Min BH. Gastric Cancer 2015)을 참고하시기 바랍니다.
En bloc resection and en bloc with R0 resection rates in MUC-EGC cases were 94.1 % and 81.7 %, respectively. MUC-EGC was significantly associated with larger tumor size, more frequent submucosal invasion, and lymphovascular invasion compared to PuD-EGC. Despite these aggressive features of MUC-EGC, no lymph node metastasis or extragastric recurrence occurred during follow-up after ESD if MUC-EGC met the curative endoscopic resection (ER) criteria for tumors of absolute or expanded indications.
[분류법 비교 - 연세대 연구]
연세대학교 강남세브란스병원 김지현 교수님팀에서 수술 환자의 병리결과를 새로운 각도로 분석한 논문이 발표되었습니다 (Yoon HJ. Pathol Res Pract 2016).
제가 흥미롭게 본 것은 ESD 적응증에 해당하는 환자의 림프절 전이 양상입니다. 자료가 축적될수록 '일부 expanded indication에서 림프절 전이가 분명히 존재한다'는 것이 명백해지고 있습니다. 3 cm 이하의 분화형 점막암에서도 궤양이 있는 경우에는 림프절 전이를 반드시 고려해야 할 것 같습니다. 점막하암은 말할 나위도 없습니다.
이 연구의 내용을 처음 본 것은 2014년 KINGCA였습니다 (링크). 당시 제가 comment 하였던 내용을 아래에 옮깁니다.
연세대학교에서 'Is new criteria for mixed histology is necessary for endoscopic resection in EGC?'라는 제목의 발표를 하였습니다. 제가 흥미롭게 본 것은 Japanese classification입니다. 우리는 흔히 일본에서 말하는 differentiated cancer는 WHO 분류로 well-differentiated와 moderately-differentiated adenocarcinoma를 합한 것과 비슷하다고 생각합니다. 그런데 이번 발표를 보니 일본 분류에서 differentiated가 49.7%인 반면 well-differentiated와 moderately-differentiated adenocarcinoma의 합은 48%였습니다. 즉 2% 차이가 있습니다. 이 환자들은 어떤 조직학적 특징인 있는지 궁금할 뿐입니다. 일본 분류를 WHO 분류와 mapping하는 일은 무척 어려운 일입니다. 2 프로 부족합니다.
한 가지 아쉬움은... 내시경 논문이자 병리 논문인데 내시경 사진이나 병리 사진이 하나도 없다는 점입니다. '이론 내시경 (theoretical endoscopy)보다는 현장 내시경(practical endoscopy)' 논문을 기대해봅니다.
2015년 연세대학교 논문입니다 (Shim CN. Surg Endosc 2015). Mixed type에 대한 병리학적 진단 기준이 명확하게 제시되지 않아서 다소 아쉬웠습니다. 결과는 명확합니다. "Mixed는 pure보다 나쁘다."
 3. Management after ESD (2020년 4월 13일 현재)
3. Management after ESD (2020년 4월 13일 현재)
ESD 후 최종 병리결과가 미분화 혼재암으로 나오면 고민이 아닐 수 없습니다. 내시경 시술 자체가 완벽하게 되었는지, 미분화 조직형의 비율이 어떠한지 등을 고민해야 하지만 일반적으로 아래와 같이 접근하고 있습니다.
(1) 미분화 혼재암, 장경 2cm 이하, 점막암, 절제 변연 음성, L/V (-/-)이면 완전절제로 보고 수술이나 항암치료 등 추가 치료 없이 경과관찰을 합니다.
(2) 미분화 혼재암이고 점막하암이면 수술을 권합니다. 혼재암이 아닌 pure한 미분화 조직형 위암에서도 점막하암이면 수술을 권합니다. SM 500um라는 기분은 분화형 위암에서만 적용하고 있습니다.
(3) 미분화 혼자암 중 (1) 점막암 2cm 초과, (2) 점막암 lateral margin positive는 애매합니다. Case-by-case로 접근합니다.
다양한 상황이 있지만 대강 아래와 같은 표준 환자설명서를 만들어 이용하고 있습니다. (2020년 4월 13일 현재)
[분화 혼재암 - 점막암, 분화형이 많은 경우]
내시경으로 절제한 조직에 대한 병리결과가 나왔습니다. 세포형, 깊이, 범위, 림프관/혈관 등에 문제가 없어야 하는데 다른 것은 큰 문제가 없고 침윤 깊이도 점막층(제1층)인데, 세포형이 내시경치료 전 조직검사와 달리 분화형과 미분화형이 섞인 혼재형으로 나왔습니다. 분화형이 미분화형에 비하여 많았습니다. 내시경 조직검사는 일부만 샘플링하여 얻은 결과이므로 전체를 대변하지 못합니다. 따라서 치료 후 세포형이 달라지는 경우가 간혹 발견됩니다.
미분화 혼재암은 흔하지 않습니다. 원래 미분화 위암은 내시경치료의 전통적인 적응증은 아니므로, 내시경 치료 후 분화형과 미분화형이 섞인 것으로 나오면 어떻게 하는 것이 최선인지 명확하지 않습니다. 과거에는 수술을 권했습니다. 그러나 수술을 해보면 잔류암이 없다고 나오는 분들이 너무 많아서 최근에는 분화형이 미분화형보다 많으면 수술보다는 조심스럽게 경과관찰을 권하는 경향(본 병원의 결과는 일본위암학회지에 보고한 바 있습니다. Gastric Cancer 2015;18:618-626)입니다. 다만 환자 수가 많지 않아서 표준화된 통일된 진료 가이드라인은 없습니다. 즉 의사간 의견이 일치되지 않았다는 말씀입니다.
물론 수술을 하게 되면 재발률을 약간 줄일 수 있다는 의견도 있습니다만 수술은 수술입니다. 위를 최소한 2/3 정도 잘라야 하고 주변 림프절까지 박리하기 때문에 수술에 따른 합병증과 수술 후 삶의 질 저하를 함께 고려해야 합니다. 전신마취의 위험도 무시할 수 없습니다. 만약 수술을 하지 않는다면 보통 조기위암 내시경치료 후 재발률을 5% 정도로 보는데 이보다 다소 높을 것이라는 정도로 이해하시면 크게 틀리지 않을 것 같습니다.
흔치 않은 애매한 경우입니다. 저희는 최대한 자세히 설명하고 환자의 선택을 존중한다는 입장을 가지고 있습니다. 이를 위하여 1주일 시간을 드리겠습니다. 충분히 생각할 시간을 가진 후 1주일 후 외래에서 환자분의 의견을 말씀해 주시기 바랍니다.
보통 2달 정도 약이 필요한데 남은 약은 충분하십니까?
계획: 1주일 후 외래에서 재상담
[미분화 혼재암 - 점막암, 미분화형이 많은 경우]
내시경으로 절제한 조직에 대한 병리결과가 나왔습니다. 세포형, 깊이, 범위, 림프관/혈관 등에 문제가 없어야 하는데 다른 것은 큰 문제가 없고 침윤 깊이도 점막층(제1층)인데, 세포형이 내시경치료 전 조직검사와 달리 분화형과 미분화형이 섞인 것으로 나왔습니다. 내시경 조직검사는 일부만 샘플링하여 얻은 결과이므로 전체를 대변하지 못합니다. 따라서 치료 후 세포형이 달라지는 경우가 간혹 발견됩니다.
환자분의 경우는 분화형에 비하여 미분화형의 비율이 높은 것으로 나왔습니다. 따라서 분화형과 미분화형으로 2분법적으로 나누면 미분화형 위암에 해당합니다. 원래 미분화 위암은 내시경치료의 전통적인 적응증은 아니므로, 내시경 치료 후 분화형과 미분화형이 섞인 것으로 나오면 어떻게 하는 것이 최선인지 명확하지 않습니다. 과거에는 수술을 권했습니다. 그러나 수술을 해보면 잔류암이 없다고 나오는 분들이 너무 많아서 최근에는 수술보다는 조심스럽게 경과관찰을 권하는 경향입니다. 다만 환자 수가 많지 않아서 표준화된 통일된 진료 가이드라인은 없습니다. 즉 의사간 의견이 일치되지 않았다는 말씀입니다.
물론 수술을 하게 되면 재발률을 약간 줄일 수 있다는 의견도 있습니다만 수술은 수술입니다. 위를 최소한 2/3 정도 잘라야 하고 주변 림프절까지 박리하기 때문에 수술에 따른 합병증과 수술 후 삶의 질 저하를 함께 고려해야 합니다. 전신마취의 위험도 무시할 수 없습니다. 만약 수술을 하지 않는다면 보통 분화형 조기위암 내시경치료 후 재발률을 5% 정도로 보는데 이보다 다소 높을 것이라는 정도로 이해하시면 크게 틀리지 않을 것 같습니다.
흔치 않은 애매한 경우입니다. 저희는 최대한 자세히 설명하고 환자의 선택을 존중한다는 입장을 가지고 있습니다. 이를 위하여 1주일 시간을 드리겠습니다. 충분히 생각할 시간을 가진 후 1주일 후 외래에서 환자분의 의견을 말씀해 주시기 바랍니다.
보통 2달 정도 약이 필요한데 남은 약은 충분하십니까?
계획: 1주일 후 외래에서 재상담
[미분화혼재암 점막하침윤]
내시경으로 절제한 조직에 대한 병리결과가 나왔습니다. 세포형, 깊이, 범위, 림프관/혈관 등에 문제가 없어야 하는데, 두 가지가 문제가 있는 것으로 나왔습니다. (1) 세포형이 분화형과 미분화형이 섞인 혼재형으로 나왔습니다. 분화형이 미분화형에 비하여 많았습니다. (2) 제1층에 국한되어 있지 않고 제2층까지 침윤된 것으로 나왔습니다.
미분화 혼재암은 흔하지 않아 통일된 진료 가이드라인이 없습니다. 의사들 사이에서도 의견이 다르다는 말씀입니다. 이는 내시경 치료 후 분화형과 미분화형이 섞인 것으로 나오면 어떻게 하는 것이 최선인지 아직 명확하지 않기 때문입니다.
미분화 혼재암으로 나오고 점막에 국한된 경우는 분화형 암과 비슷하게 접근하는 것이 보통입니다. 대부분의 의사가 수술보다는 경과관찰을 선택한다는 것입니다. 그러나 미분화 혼재암이 점막하층까지 침윤되어 있으면 재발 위험이 높아집니다. 따라서 수술을 권하는 의사가 많습니다. 저도 수술을 권하고 싶습니다.
병리결과에 문제가 없을 때 재발률이 5% 정도인데 반하여, 현재의 재발 위험은 10-20% 이상입니다. 만약 재발하면 절반 이상은 완치의 기회가 없습니다. 따라서 수술이 경과관찰보다 유리한 상황입니다. 물론 수술은 수술입니다. 전신마취에 따른 위험, 통증, 수술의 합병증, 수술 후 삶의 질 저하 등의 어려운 점이 있지만 그래도 재발위험을 더 많이 고려해야 한다고 판단됩니다. 현재 암이 남아있다는 증거가 있어 수술을 권하는 것은 아닙니다. 단지 재발위험이 높기 때문입니다. 수술을 해보면 눈에 보일 정도의 암이 남아있는 경우는 10-20% 정도입니다. 이러한 내용을 모두 종합하여 판단할 때 수술을 권하고 싶습니다.
흔치 않은 애매한 경우입니다. 이럴 때에는 최대한 자세히 설명하고 환자의 의견을 존중하는 수 밖에 없습니다. 오늘 내일 사이에 최종 의견을 주셔도 좋고 1주일 정도 후 외래에서 의견을 주셔도 좋습니다. 의료진 사이에서도 의견이 다양하므로 2차 의견을 들어보셔도 좋습니다.
보통 2달 정도 약이 필요한데 남은 약은 충분하십니까?
계획: 1주일 후 외래에서 재상담
[혼재암 (미분화 90%), 점막암, 28mm]
내시경으로 절제한 조직에 대한 병리결과가 나왔습니다. 세포형, 깊이, 범위, 림프관/혈관 등 모두 문제가 없어야 하는데 몇 가지 우려점이 나왔습니다. 일전 타 병원 EUS에서 점막하층 침윤이 의심되었는데 최종 병리결과는 점막암(제1층)으로 나온 점은 그나마 다행스러운 부분입니다. 그런데 세포형은 예상했던 바와 같이 분화형과 미분화형이 섞여 있는 것으로 나왔고, 그 비율은 분화형(10%)에 비하여 미분화형이 훨씬 많았습니다. 그리고 위암의 최종크기가 28mm로 나왔습니다. 수술을 권하는 상황입니다.
과거에는 미분화형은 무조건 수술을 권했습니다. 최근에는 환자께서 강력히 원하시면 내시경치료를 하기도 합니다. 다만 조건이 있습니다. 최종 병리결과 미분화암이 점막에 국한되어 있고 크기가 2cm 보다 작아야 한다는 것입니다. 환자분의 경우는 크기 기준 초과입니다.
일반적으로 수술을 하면 재발률을 줄일 수 있습니다. 다만 수술은 수술이라는 점이 걱정입니다. 위를 2/3 정도 잘라야 하고 주변 림프절까지 박리하기 때문에 수술에 따른 합병증과 수술 후 삶의 질 저하를 함께 고려하지 않을 수 없습니다. 전신마취의 위험도 무시할 수 없습니다. 만약 수술을 하지 않는다면 보통 분화형 조기위암 내시경치료 후 재발률을 5% 정도로 보는데, 환자분의 경우는 이보다 다소 높습니다. 비록 정확한 예측 방법은 확립되어있지 않지만 대략 10-20% 수준일 것으로 판단됩니다.
일단 외과의뢰를 하겠습니다. 우리말로 자세히 써 두었으니 의무기록을 복사하여 다시 한번 가족들과 상세히 읽어보시고, 외과 선생님의 의견을 들으시기 바랍니다. 혹시 추가로 상담할 사항이 있을지 모르므로 1주일 후 제 외래를 잡아놓겠습니다.
수술 전까지는 약을 드셔야 합니다. 남은 약은 충분할 것입니다.
계획 1: 의무기록 복사
계획 2: 외과 의뢰 (위암 내시경 치료 후 미분화형 점막암 28mm로 나왔습니다. 미분화암의 병리학적 완전절제 기준인 20mm를 초과하였으므로 귀과적 치료를 위하여 의뢰드립니다.)
계획 3: 1주일 후 소화기내과 외래 (추가 상담이 필요한 경우에만 방문하시면 됩니다)
ESD를 하였습니다. 아래와 같은 결과였습니다. 여러분은 무엇을 권하겠습니다. 수술 혹은 경과관찰 중 무엇을?
Stomach, endoscopic submucosal dissection:
Early gastric carcinoma
1. Location : antrum, greater curvature
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated > poorly differentiated (30 %)
4. Histologic type by Lauren : mixed
5. Size of carcinoma : (1) longest diameter, 38 mm (2) vertical diameter, 30 mm
6. Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
7. Resection margin : free from carcinoma(N)
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: present
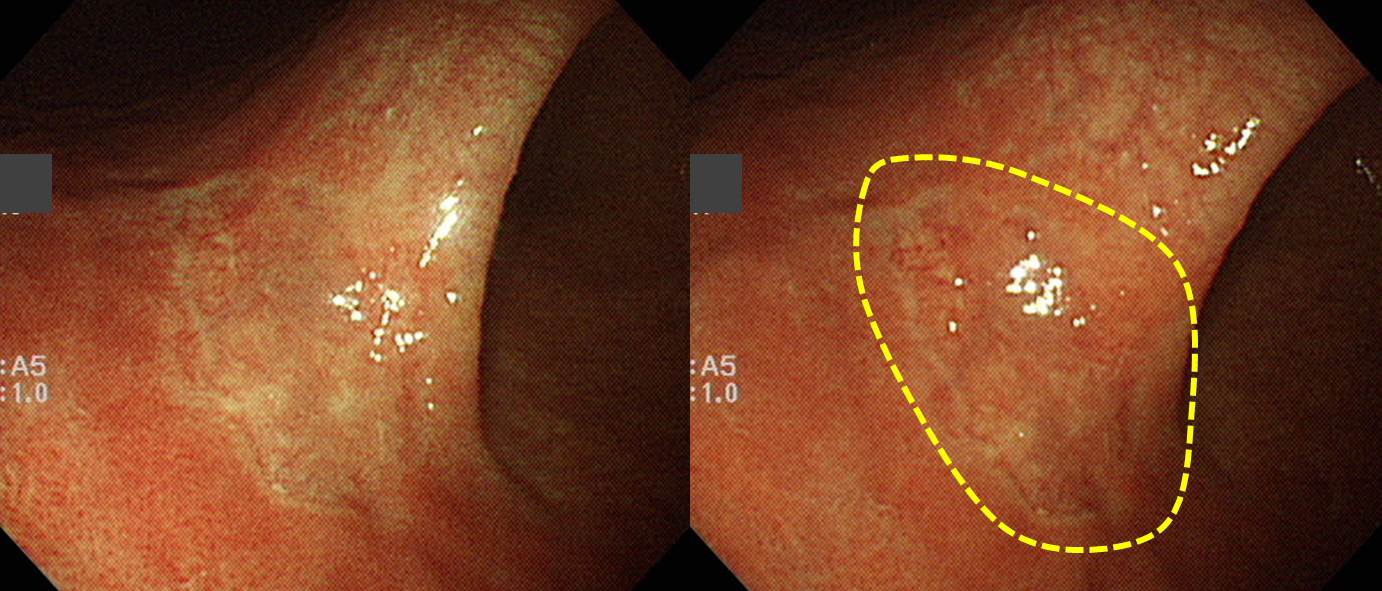
60대 여성입니다. 조직검사는 M/D adenocarcinoma였습니다. 어떤 치료법을 선택하시겠습니까? (위암 493)
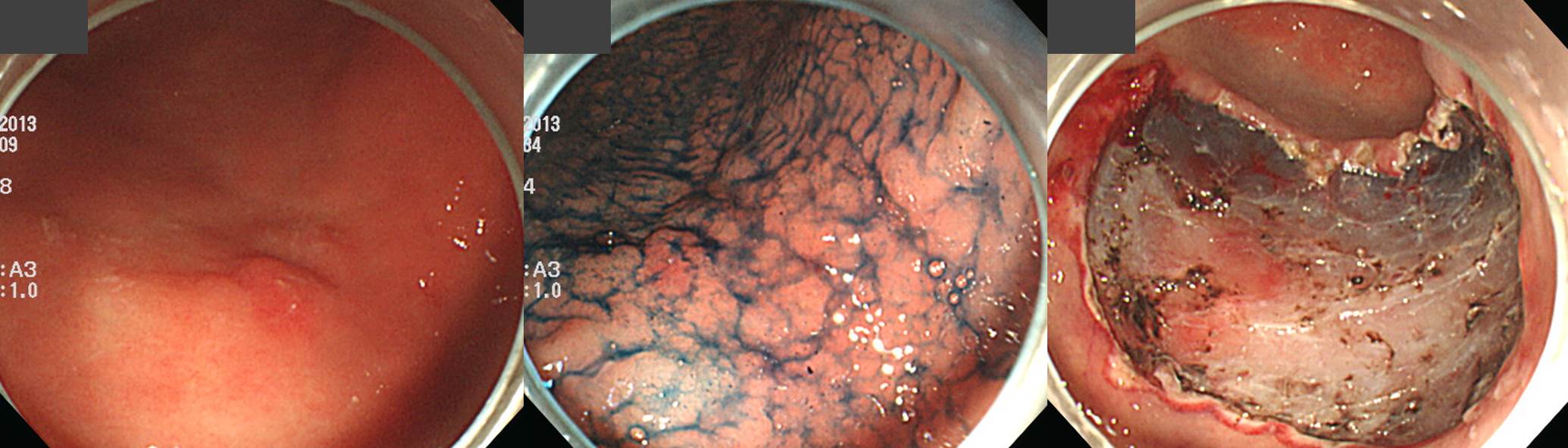
IIc + IIa 형이므로 점막하암일 가능성이 제법 있는 상황이지만 일단 ESD를 하고 최종 병리결과 의거 수술 필요 여부를 결정하기로 하였습니다.
다소 우려하였던 바와 같이 점막하암으로 나왔습니다. 깊이는 500 um, 미분화 혼재암으로 나왔습니다. 수술을 권하시겠습니까, 경과관찰을 하시겠습니까?
1. Stomach, #1x1 : GC of low body, endoscopic submucosal dissection:
. Early gastric carcinoma
1. Location : body, greater curvature
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated >> tubular adenocarcinoma, poorly differentiated (about 15%)
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 24 mm (2) vertical diameter, 13 mm
6. Depth of invasion : invades submucosa, (depth of sm invasion : 500 ㎛) (pT1b)
7. Resection margin : free from carcinoma(N) safety margin : distal 7 mm, proximal 9 mm, anterior 10 mm, posterior 8 mm, deep 400㎛ (sm only)
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: present
저는 아래와 같이 설명하고 수술을 권했습니다.
내시경 시술 후 최종 병리결과를 확인하기 위한 외래 방문입니다. 비교적 작은 조기위암으로 판단되어 85% 정도의 초기성공률 (내시경치료만으로 일차 치료가 끝나는 비율)을 예측하는 상황에서 내시경치료를 하였는데, 아쉽게도 그 85%에 들지 못하고 수술이 필요한 15%에 해당하는 결과가 나왔습니다. 내시경으로 절제한 표본에 대한 최종 병리결과에서 세포형, 깊이, 범위, 림프관/혈관에 모두 문제가 없어야 하는데 아쉽게도 문제가 있는 것으로 나왔습니다. 크기는 24밀리로 예상한 것을 크게 벗어나지 않았는데 제 2층까지 침윤되어 있고 미분화요소 가 15% 섞여 있었습니다. 즉 수술이 필요한 것으로 나왔습니다. 이런 분들이 약 15%정도 됩니다.
병리결과에 문제가 없을 때 재발률이 5% 정도인데 반하여, 현재의 재발 위험은 10-20% 이상입니다. 만약 재발하면 절반 이상은 완치의 기회가 없습니다 .따라서 수술이 경과관찰보다 유리한 상황입니다. 물론 수술은 수술입니다. 전신마취에 따른 위험, 통증, 수술의 합병증, 수술 후 삶의 질 저하 등의 어려운 점이 있지만 그래도 재발위험을 더 많이 고려해야 한다고 판단됩니다. 현재 암이 남아있다는 증거가 있어 수술을 권하는 것은 아닙니다. 단지 재발위험이 높기 때문입니다. 수술을 해보면 눈에 보일 정도의 암이 남아있는 경우는 10-20% 정도입니다. 이러한 내용을 모두 종합하여 판단할 때 수술을 권하고 싶습니다.
위암 603
Stomach, ESD : Early gastric carcinoma
1. Location : body, lesser curvature
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated >> poorly differentiated (30%)
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 24 mm (2) vertical diameter, 8 mm
6. Depth of invasion : invades mucosa (lamina propria) (pT1a)
7. Resection margin : free from carcinoma(N), safety margin : distal 12 mm, proximal 7 mm, anterior 6 mm, posterior 18 mm, deep 400 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: present
Initial biopsy: P/D
Stomach, subtotal gastrectomy: Early gastric carcinoma
1. Location : middle third, Center at low body and anterior wall
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated with poorly differentiated component (10%)
4. Histologic type by Lauren : mixed
5. Size : 2.1x1.5 cm
6. Depth of invasion : invades mucosa (muscularis mucosae) (pT1a)
7. Resection margin: free from carcinoma, safety margin: proximal 1.4 cm, distal 9.8 cm
8. Lymph node metastasis : no metastasis in 62 regional lymph nodes (pN0) (0/62 : "3", 0/7; "4", 0/13; "5", 0/8; "6", 0/5; "7", 0/4; "9", 0/5; "8a", 0/4; "11p", 0/3; "12a", 0/0; "4sb", 0/3; "1", 0/0)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. AJCC stage by 7th edition: pT1a N0
Stomach, subtotal gastrectomy: Early gastric carcinoma
1. Location : lower third, Center at body and anterior wall
2. Gross type : EGC type IIb
3. Histologic type : tubular adenocarcinoma, moderately differentiated > poorly differentiated (30%)
4. Histologic type by Lauren : mixed
5. Size : 3x1.8 cm
6. Depth of invasion : invades mucosa (muscularis mucosae) (pT1a)
7. Resection margin: free from carcinoma, safety margin: proximal 1.8 cm, distal 6.9 cm
8. Lymph node metastasis : no metastasis in 37 regional lymph nodes (pN0) (0/37 : "3", 0/14; "4", 0/4; "5", 0/0; "6", 0/7; "7", 0/3; "9", 0/1; "8a", 0/1; "11p", 0/0; "12a", 0/3; "4sb", 0/1; "1", 0/3)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. AJCC stage by 7th edition: pT1a N0
위암 540
Stomach, subtotal gastrectomy: Early gastric carcinoma
1. Location : lower third. Center at mid antrum and lesser curvature
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated >> poorly differentiated (20%)
4. Histologic type by Lauren : mixed
5. Size : 1.4x1.0 cm
6. Depth of invasion : invades submucosa (sm3) (pT1b)
7. Resection margin: free from carcinoma, safety margin: proximal 4.7 cm, distal 2.2 cm
8. Lymph node metastasis : no metastasis in 44 regional lymph nodes (pN0)
9. Lymphatic invasion : present
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. AJCC stage by 7th edition: pT1b N0
(2016) 이 환자에 대한 보다 자세한 설명은 위암 615를 보십시오
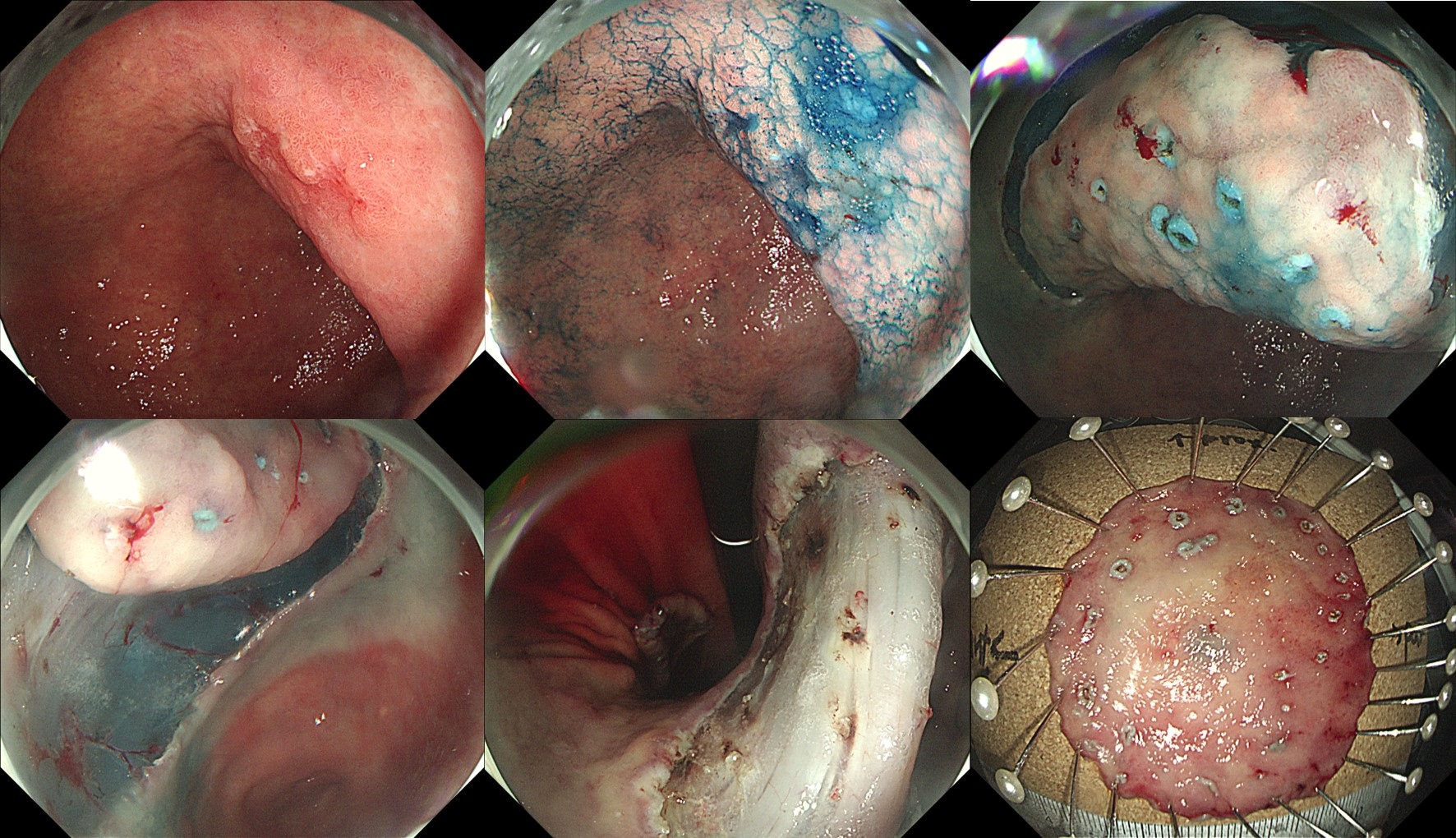
LC of distal antrum, ESD : Early gastric carcinoma
1. Location : distal antrum, lesser curvature
2. Gross type : EGC type IIa+IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated >> tubular adenocarcinoma, poorly differentiated (30%)
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 18 mm (2) vertical diameter, 9 mm
6. Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
7. Resection margin : free from carcinoma(N), safety margin : distal 8 mm, proximal 8 mm, anterior 8 mm, posterior 16 mm, deep 1200 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: present
The rate of pathological non-curative resection of EGC by ESD is about 10-20%. In additional surgery for non-curative resection cases, local residual tumor is found in 5-10%, and lymph node metastasis is also found in 5-10%. In this case of histological heterogeneity, lateral margin was involved. Surgery was done and 1.2cm x 0.3cm sized residual tumor in lamina propria was found. (EndoTODAY 위암 650)
[2018-7-28. 애독자 질문]
미분화 혼재암 ESD 후 절제변연 양성으로 수술을 권한 증례(EndoTODAY 위암 650)에 대한 질문입니다. Mixed type 의 경우 악성의 가능성이 더 높다고 하신 바 있습니다 (Shim CN. Surg Endosc 2015). 일전에 보여주신 환자설명자료(EndoTODAY 위암 615)에서는 '최근에는 혼재형에서도 ESD를 할 수 있다'고 하셨기에 조금 혼란스럽습니다.
[2018-7-28. 이준행 답변]
위암을 조직형에 따라 분화형과 미분화형으로 나누는 것은 엄밀한 방법은 아니지만, 편리한 측면이 있어서 ESD 영역에서 종종 사용되고 있습니다. 분화형과 미분화형이 섞인 미분화 혼재암은 아직 그 정의조차 명확하지 않습니다. Histological heterogeneity라고 표현되기도 합니다. 같은 말입니다.
미분화 혼재암이 분화조직형보다 나쁜 것은 틀림없습니다. 그런데, 미분화 혼재암을 순수한 미분화 조직형 암과 비교하면 어떨까요? 직관적으로는 미분화 혼재형은 분화조직형과 미분화조직형의 중간 정도일 것 같지만, 연구 결과는 섞인 것은 순순한 것보다 나쁘다는 것입니다 (Shim CN. Surg Endosc 2015). 저도 미분화 혼재암은 순수한 미분화 조직형 (P/D 혹은 SRC) 위암보다 비슷하거나 더 나쁠 것으로 생각하고 있습니다.
내시경 육안 소견이 분화조직형 위암에 가까운데 조직검사에서 mixed type으로 나오면 조심스럽게 ESD를 시행할 수 있습니다. 물론 크기 기준을 엄격하게 적용합니다. 1-2cm 이상에서는 절대 시행하지 않는 것이지요.
임상에서는 ESD 전 조직검사에서는 분화조직형 위암으로 나왔는데 ESD 후 최종 병리결과가 미분화 혼재형으로 나온 경우가 많습니다.
(1) 미분화 혼재암이더라도 점막암이고 (2cm 이하이면서) 절제 변연이 음성이면 완전절제로 간주하고 경과관찰을 합니다.
(2) 미분화 혼재암이고 점막하암이면 수술하는 경우가 많습니다. 이 부분은 다소 논란이 있어 case by case로 접근합니다. 일반적인 curative resection criteria에 만족하면 경과관찰을 하기도 합니다.
(3) 문제는 미분화 혼재암이고 절제 변연이 양성인 경우입니다. 분화조직형 위암에 절제변연이 양성이면 추가 절제술을 하거나, 소작술을 하거나, 조심스럽게 경과관찰을 할 수 있습니다. 미분화 혼재암에서 절제 변연이 양성이면 residual tumor의 가능성이 높습니다. 미분화 혼재암은 내시경 육안소견으로 위암의 경계를 명확히 확인하기 어렵고, ESD 후 multiple lateral margin involvement가 자주 발견됩니다 (Lee JH. Surg Endosc 2015). 저는 미분화 혼재암인데 절제변연이 양성이면, 특히 미분화암이 절제변연에서 발견되면 수술을 권하고 있습니다. 문의하신 EndoTODA 위암 650의 병리결과를 보면 "involvement of proximal margin by carcinoma (poorly differentiated)"라는 부분이 있었습니다. 수술 후 최종 병리에서도 residual tumor가 있는 것으로 나와서 수술을 권하길 잘 했다고 생각하였습니다.
저와 함께 일하고 있는 민병훈 교수께서 삼성서울병원의 미분화 혼재암 ESD 성적에 대하여 보고한 바 있으니 참고하시기 바랍니다 (Min BH. Gastric Cancer 2015).
Min. 2015
En bloc resection and en bloc with R0 resection rates in MUC-EGC cases were 94.1 % and 81.7 %, respectively. MUC-EGC was significantly associated with larger tumor size, more frequent submucosal invasion, and lymphovascular invasion compared to PuD-EGC. Despite these aggressive features of MUC-EGC, no lymph node metastasis or extragastric recurrence occurred during follow-up after ESD if MUC-EGC met the curative endoscopic resection (ER) criteria for tumors of absolute or expanded indications.
교수님의 가르침 덕분에 ESD를 열심히 하고 있습니다. 저번 달에 5개를 했는데 antrum은 안 오고 body랑 angle만 와서 처음에는 많이 힘들었는데, 그래도 조금씩 나아지는 것 같아 다행입니다. 1년 동안 교수님 옆에서 본 덕분에 ESD 하면서 머리가 아닌 몸이 먼저 움직이고 있더라고요..ㅎㅎ
최근 EndoTODAY에 mixed adenocarcinoma에 대한 포스팅을 봤는데, 저도 어떻게 해야할 지 고민이라 조언을 구하고자 합니다. 70세 여자로 직장암과 뇌출혈의 병력이 있는 분으로 LC of LB에 1.5cm 정도되는 IIa+IIc 병변이 있어 ESD 시행하였습니다.
Stomach, angle, endoscopic submucosal dissection: MIXED ADENOCARCINOMA (Tubular adenocarcinoma, moderately differentiated, 60%, Poorly cohesive carcinoma, 20%, and Mucinous adenocarcinoma, 20%)
1) Size: about 1.59 x 0.83 cm
2) Invades into the mucosa and muscularis mucosa
3) Depth: Total tumor depth: 0.07 cm, No submucosal invasion
4) Lymphovascular invasion: not present
5) Resection margin: free from the tumor
- Distance from the closest lateral margin: 1.31 cm
- Distance from the closest deep margin: 0.03 cm
Immnohistochemical stain: p53: (-), Aberrant expression, HER2 (c-erbB2): (Negative, -), MLH-1 (+)MM까지만 침범했고, 수술을 하기에는 고령 및 underlying diseases가 있어 close observation을 하려고 하는데, 괜찮을까요?
[2019-5-13. 이준행 답변]
안녕하십니까.
ESD 후 최종 병리결과 미분화 혼재암(mixed, histological heterogeneity)으로 나오면 늘 고민입니다. 순수하게 미분화 조직형 위암이고 2cm 이하이고 점막암이면 추가 치료 없이 경과관찰을 하는데, 미분화 혼재암의 경우는 순순한 미분화 조직형암 위암에 비하여 좀 더 aggressive하다는 연구 결과(Shim CN. Surg Endosc 2015)도 있어서 고민하지 않을 수 없습니다. 2018년 한 애독자 질문과 답변을 보시면 저의 접근법을 보실 수 있을 것입니다. 다시 말쓰드리면...
(1) 미분화 혼재암, 장경 2cm 이하, 점막암, 절제 변연 음성, L/V (-/-)이면 완전절제로 보고 경과관찰을 합니다.
(2) 미분화 혼재암이고 점막하암이면 수술을 권합니다. 혼재암이 아닌 pure한 미분화 조직형 위암에서도 점막하암이면 수술을 권합니다. SM 500um라는 기분은 분화형 위암에서만 적용하고 있습니다.
(3) 미분화 혼재암 중 (1) 점막암 2cm 초과, (2) 점막암 lateral margin positive는 애매합니다. Case-by-case로 접근하고 있습니다.
이러한 기준에 따르면 비록 미분화 혼재암이지만 깔끔한 내시경 시술이 되었고, 점막암이고, 2cm 이하이고, 다른 재발 위험이 없으므로 환자의 건강상태와 무관하게 수술이나 항암치료 등 추가치료가 필요하지 않다고 생각합니다. 특히 문의하신 환자는 고령이고 타장기 질환도 있으므로 더욱 그러합니다. Primary cancer 재발과 metachronous cancer를 포함하여 대강 5년 5% 재발률을 예상하는 상태에서 경과관찰 할 수 있다고 생각합니다.
2) 위암 615 - 미분화 혼재암 ESD에 대한 시술 전후 환자 설명
3) 위암 644 - ESD 후 최종 병리결과에서 여러 위험인자가 있는 환자에게 어떻게 설명할 것인가? Minute SM invasion and histological heterogeneity
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.