 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [위내시경 질지표. Quality indicators of EGD] - 終
[위내시경 질지표. Quality indicators of EGD] - 終
2005년 국군광주병원 노충국 병장 사건읕 통하여 위내시경 검사 quality에 대한 중대한 문제제기가 있었습니다. 그럼에도 불구하고 우리나라 내시경의 질향상을 위한 여정은 험하기만 합니다. 기초 교육도 제대로 되지 않고 있으니...
1. 위내시경 질지표
4. 내시경 검사 건수
5. Missing rate for gastric cancer
7. [2023-5-8. 한국경제TV] 위내시경 받았는데 위암?…"의사가 3분 이상 관찰해야"
8. Cases
9. FAQs
10. References
2018-12-1. 을지병원 심포지엄. 내시경 질지표에 시간 개념이 들어가야 한다고 주장하였습니다. 위내시경의 최소 검사시간은 5분입니다.
여러 기관에서 제시한 질지표를 안용환 원장님께서 정리 (키메디에서 동영상 보기)
2022년 Post-Endoscopy Upper Gastrointestinal Cancers에 대한 Gastroenterology 논문은 이런 문장으로 시작합니다. 어마어마하게 많이 놓치고 있다는 말입니다. 물론 이유가 있습니다만...
Ten percent of patients with an upper gastrointestinal cancer will have received an esophagogastroduodenoscopy (EGD) within 3 years before diagnosis, termed post-endoscopy upper gastrointestinal cancers (PEUGIC).
[2017-3-4. 애독자 질문]
하부내시경의 질 평가 시 사용되는 adenoma detection rate와 같은 척도가 상부 내시경에도 있는가 하는 것입니다. 제 짧은 소견으로는, 작으면서도 의미있는 병소를 잘 찾아내는 내시경 의사가 좋은 내시경 의사가 아닐까 생각하고 있습니다. 그래서 "의미있는 작은 병소를 찾은 비율 = 찾아낸 의미있는 병소 수 / 내시경 시행 횟수"로 정의할 기준이 있는지 알고싶습니다.
[2017-3-4. 이준행 답변]
대장내시경에서는 adenoma detection rate나 colonoscopy withdrawal time과 같은 유명한 지표가 있습니다 (EndoTODAY 20131117). Colonoscopy withdrawal time과 adenoma detection rate의 관계는 명백하고 (Barclay RL. NEJM 2006), adenoma detection rate와 interval cancer 발생률 사이의 연관관계도 입증되었습니다 (Kaminski MF. NEJM 2010). 그러나 위내시경에서는 직관적이고 입증가능한 유용한 질지표가 개발되지 않았습니다.
의료에서의 질지표는 (1) structure 지표, (2) process 지표, (3) outcome 지표가 있습니다. 가장 직관적인 것은 outcome 지표이고, 다음은 outcome과 관련성이 입증된 process 지표입니다. 대장내시경 영역에는 outcome 지표인 adenoma detection rate와 outcome과 관련성이 입증된 process 지표인 withdrawal time이라는 직관적이고 쉽게 측정할 수 있는 것들이 있기 때문에 누구나 동의하고 쉽게 받아들일 수 있는 것입니다. 그런데 위내시경에서는 그런 것들이 없습니다.
우리나라에서 흔히 언급되고 있는 것은 '국가암검진 위내시경 질 평가 항목'입니다 (차재명. 소화기내시경 질 평가 항목: 문제점과 개선 방향). Stucture 지표와 process 지표뿐이고 outcome 지표는 없습니다.
미국내시경학회에서 2015년 Quality indicators for EGD를 발표한 바 있습니다. 위내시경에 대해서는 22개의 지표가 제시되었는데 몽땅 process 지표입니다 (Table 4). Outcome 지표가 하나도 없었습니다. 22개 중 중요한 것 4개를 선정하여 따로 제시하였는데 (Table 5), 모두 궤양에 관한 process 지표였습니다. 우리나라에서 관심있는 위암 관련 지표는 하나도 없었습니다. 그러니 위암 진단이 위내시경의 최대 목적인 우리 실정에는 전혀 적합하지 않은 지표인 셈입니다.
유럽내시경학회에서도 2016년 Performance measures for upper GI 를 발표하였습니다. 이 또한 몽땅 process 지표였습니다.
제가 유럽의 위내시경 질지표에서 관심있게 본 것은 첫 내시경 검사와 장상피화생 추적관찰에서 검사시간(intubation에서 extubation까지)이 7분은 되어야 한다는 것이었습니다 ("Percentage of first-time gastroscopies and follow-up gastroscopies for gastric intestinal metaplasia lasting more than seven minutes from intubation to extubation"). 현재 저의 위내시경 검사 시간은 보통 4-5분입니다. 유럽 질지표의 정의를 보면서 앞으로는 조금 더 오래 검사해야 하는지 고민하게 되었습니다.
저는 우리나라에서 제안된 국가암검진 위내시경 질 평가 항목이 비교적 타당하다고 생각합니다. 검사시간 7분은 우리나라 현실에서 너무 어려운 일입니다만, 5분 정도는 필요할 것 같습니다. Adenoma detection rate나 cancer detection rate는 측정하면 좋겠지만, 평가를 위한 근거 자료가 없다는 점이 문제입니다. 우리나라 검진 내시경에서 보통 300-500명 검사하면 1명에서 위암이 발견되고 있다는 점을 고려하여 각자 스스로 혹은 기관차원에서 검사 건수 대비 위암 발견율을 모니터링하면 좋을 것 같습니다.
질향상 노력은 어렵습니다. William A. Foster는 이렇게 말했다고 합니다. "Quality is never an accident; it is always the result of high intention, sincere effort, intelligent direction, and skillful execution; it represents the wise choice of many alternatives."
[2017-3-5. 경희대학교 차재명 교수님 편지]
위내시경 검사 시간에 대하여 최근 일본에서는 7분이 적당한 것 같다는 의견이 새롭게 제시되었습니다 (Kawamura T. Dig Endosc 2017). 이 연구에서는 평균 검사시간이 6.2분였는데, 5분 미만으로 검사하는 의사들에 비해 6-7분 검사하는 의사, 7분 이상 검사하는 의사들이 유의하게 더 많은 병변을 찾아내고 있었습니다.
Results: Mean examination time of 13 661 EGD without biopsy was 6.2 min (range, 2-18 min). When cut-off times of 5 and 7 min were used, four endoscopists were classified into the fast (mean duration, 4.4 ± 1.0 min), 12 into the moderate (6.1 ± 1.4 min), and four into the slow (7.8 ± 1.9 min) groups. Neoplastic lesion detection rates in the fast, moderate, and slow groups were 0.57% (13/2288), 0.97% (99/10 180), and 0.94% (31/3295), respectively. Compared with that in the fast group, odds ratios for the neoplastic lesion detection rate in the moderate and slow groups were 1.90 (95% confidence interval [CI], 1.06-3.40) and 1.89 (95% CI, 0.98-3.64), respectively.
대장내시경에서 CRC (colorectal cancer)보다 ADR (adenoma detection rate)을 타겟으로 삼고 있는 것은 CRC가 목표이지만, 빈도가 드물기 때문에 ADR을 타겟으로 삼는 것입니다. 위암에서는 adenoma-carcinoma와 같이 분명한 전암성 병변을 정하기 어렵기 때문에, ADR과 같은 타겟을 발굴하기 어렵습니다. 위의 adenoma는 대장의 adenoma와 빈도와 의미가 전혀 다르 기 때문에 위에서 ADR을 사용할 수도 없습니다.
위암 발견율보다는 전암성 병변을 병리학적 진단 목표로 제시하는 것이 바람직하지만, 위암의 암화 경로가 다양하고 위축성 위염이나 장상피화생 변화를 찾아내더라도 위암으로의 진행을 예방할 수 있는 방법이 없기 때문에 어떤 전암성 병변을 목표로 설정해야할 지 애매한 면이 있습니다. 향후 해결되어야 할 큰 숙제 같은 느낌입니다.
[2017-3-5. 이준행 답변]
차재명 교수님. 좋은 의견 감사합니다. 위내시경에서 adenoma detection rate를 적용할 수 없는 이유를 잘 설명해 주셨습니다.
위내시경 검사 시간 이슈는 참 어렵습니다. 물론 오래보면 오래 볼수록 neoplastic lesion을 많이 찾을 수 있을 것입니다. 그러나 무조건 많은 것이 좋은 것은 아닙니다.
1) 만약 오래 관찰하여 추가로 발견되는 것들이 대부분 2-3mm 저도선종이라면 꼭 긴 검사가 좋은 검사라고 말하지 못할 수 있습니다. 대장에서는 2-3mm 저도선종이 발견되면 그 자리에서 조직검사로 제거하기 때문에 추가 처치가 필요하지 않습니다. 훨씬 더 큰 선종도 one stage polypectomy로 그 자리에서 바로 제거합니다. 그러나 위에서는 병소의 경계가 명확하지 않고 주변에 염증이 있기 마련이므로 대부분의 경우 조직검사로 제거되었다는 표현을 사용하지 않고 있습니다. 위 선종을 one stage endoscopic resection을 할 수도 없습니다. 따라서 위 조직검사에서 neoplastic lesion이 나오면 거의 항상 뭔가를 더 해야만 하는 상황에 처합니다. 이에 따른 비용과 위험도 함께 고려되어야 합니다.
2) 위내시경으로 진단되지 못하여 임상적으로 문제가 되는 것은 보만 4형 진행성 위암이나 blind area에 위치한 (진행성) 위암입니다. 이는 오래 본다고 찾아지는 것이 아닙니다. 4-5분이면 충분합니다. 검사 시간보다는 지식과 경험이 부족하고 좋은 검사 방법("decent endoscopic routine")을 배우고 익히지 못하였기 때문입니다. 내시경 교육 부족을 긴 검사시간으로 대체할 수 없습니다. 경험과 지식이 부족한 상태에서 지나치게 오래 검사하면 별다른 임상적 의의가 없는 병소를 너무 상세히 기술하고 불필요하게 많은 조직검사로 연결되어 이상한 경과로 이어지는 경우도 있습니다. 사실 충분한 내시경 교육을 받지 못한 분들의 검사시간이 더 짧은 경우도 있습니다. 잘 배운 분들은 대강 어느 정도 적당한 시간 검사를 하는데 반하여, 잘 배우지 못한 분들은 너무 짧게 하거나 너무 길게 하는 등 표준화가 되어 있지 못합니다. 요컨데 내시경 교육 이슈가 더 중요하다고 생각합니다.
3) 현실적인 고려점도 있습니다. 위내시경은 대장내시경에 비하여 더 자주 받아야 합니다. 진정내시경이 아닌 경우도 많습니다. 검사시간이 너무 길면 환자들이 지쳐서 다음 검사를 꺼려하는 경우도 있습니다. 사실 많습니다. 힘든 검사 후 "죽으면 죽었지 다시는 검사받지 않겠다"고 다짐하는 환자도 있으니까요.
요컨데, 위내시경에서도 검사시간이 길면 뭔가 더 발견할 수 있는 것은 사실이지만 표준 검사 시간을 지나치게 늘릴 근거는 부족한 것 같습니다. 충분한 내시경 교육을 받은 분들이라면 5분 정도의 검사시간이면 acceptable하다고 생각됩니다. 환자의 기본 정보를 확인하고, 진정제를 투약하고, 검사 기록을 남기는 것까지 고려하면 한 시간에 5명 정도의 검사가 maximum입니다.
우리나라에서 위내시경 질관리의 핵심은 '내시경 교육 훈련'과 '내시경 검사 시간 5분'이라고 생각합니다. 좋은 의견 감사합니다.
[2021-2-25] Endoscopy education conference organized by Pentax
Pentax 사의 내시경 교육 webinar에 참석하여 삼성서울병원의 BOXIM 프로그램을 소개하였습니다. 아산병원 김도훈 교수님과 경북대 전성우 교수님의 멋진 강의도 있었습니다. 풍납동과 대구에서 내시경 tutoring 방법이 급속히 발전하고 있는 모습이 인상적이었습니다.아산병원 내시경 교육 프로그램 중 위내시경 검사 시간이 언급된 부분이 있어 소개합니다. 아산병원에서도 5분 - 5분 30초 검사하도록 가르치고 있습니다. 그렇습니다. 위내시경은 최소한 5분은 검사해야 합니다. 5분.
Longer observation time increases the detection rate of neoplasms in EGC: a quality indicator study 가톨릭대학교 박재명 (2017-4-8. 한일헬리코박터 학회)
A higher neoplasm detection rate was found among endoscopists who had a longer mean examination time during EGD.
[이준행 한마디] 건진 위내시경에서 검사시간이 길수록, 조직검사를 많이 할수르고 종양을 많이 발견한다는 데이타이며, multivariate analysis에서 검사 시간이 중요한 quality indicator였습니다. 매우 중요한 자료가 아닐 수 없습니다. 다만 우려스러운 것은 너무 많은 조직검사입니다. 내시경 조직검사가 6.9-27.8%의 환자에서 시행되었고, 종양은 0.14-0.32%에서 발견되었습니다. 대강 100개 조직검사에서 1개 종양이 나왔다는 이야기입니다. 저의 임상 경험으로 판단하면 조직검사 중 1%에서 종양이 나왔다는 것은 너무 낮은 수치인 것 같습니다. 건진 위내시경에서 조직검사의 threshold가 너무 낮은 것은 아닌지 우려됩니다. 이 부분에 대하여 좀 더 살펴볼 필요가 있을 것 같습니다.
이 자료는 Gastroenterology 2017년에 발표되었습니다.
박교수께서는 내시경 시행하는 의사의 태도를 중요하게 언급하셨습니다. 귀무가설이라는 개념으로 설명하셨는데요... "모든 환자에서 암이 있다고 가정하고 검사를 합시다. 암이 없으면 다시 관찰해야 합니다."라고 말씀하신 부분은 정말 옳은 이야기라고 생각되었습니다.
3년을 기준으로 했다는 점이 너무 가혹한 것 같습니다만... Nat Rev Gastroenterol Hepatol. 2015)
조직검사와 암 발견율의 관련성은 우리나라와 외국에서 모두 입증되었습니다.
대장에서 endocytoscopy를 이용한 AI가 도움이 된다는 신선한 연구입니다.
Cecum intubation rate와 비슷한 것이 ampulla of Vater 관찰률인데 ampulla of Vater를 자세히 본 의사가 십이지장과 위 종양 진단율이 높아집니다.
위점막은 최소한 2번 이상 보도록 권하고 있다고 하십니다.
보는 것이 더 중요하고 많은 사진 남기는 것 보다 필요한 것만큼 찍는 것이 중요하지 않을까 생각됩니다.
박재명 교수님은 관찰 시간의 중요성를 강조하면서 qaulity improvement에 대한 멋진 강의를 마치셨습니다. 관찰시간을 1분 늘렸더니 종양 진단율이 거의 50% 증가된다는 멋진 경험을 소개해 주셨습니다.
객관적 질지표: (1) 충분한 시간, (2) Protocol, (3) Biopsy rate, (4) 구조물 촬영
주관적 질지표: (1) 종양이 있다는 귀무가설로 검사를 하자, (2) 맹점을 인식하자, (3) 나의 경험을 너무 믿지 말자, (4) 내시경 실력을 키우자. 색조 변화와 공기 주입 등
"매일 같이 이 경전을 암송하는 이에게 생명의 빛이 있으리라."
우측 그래프를 잘 보면 좋을 것 같습니다. 조직검사를 많이하면 주로 atrophy나 metaplasia와 같은 premalignant condition을 높이지만 dysplasia나 cancer는 아주 조금 더 발견할 수 있을 뿐입니다. 조직검사를 하기 전에 잘 보는 것이 더 중요할지 모르겠습니다. 조직검사를 너무 많이 하면 합병증이 증가될 수 있고 내시경실을 효율성이 낮아집니다.
 [2022-5] 박재명 교수님 review (Clinical Endoscopy 2022년 5월호)
[2022-5] 박재명 교수님 review (Clinical Endoscopy 2022년 5월호)
"To date, no qualified on-site training center exist in Korea."라는 부분이 안타까웠습니다. 학회와 같은 공식적인 기관에서 on-site training center를 만들고 운영하면 좋을 것 같습니다. 현재까지는 삼성서울병원 임상시뮬레이션센터의 BOXIM program을 이용하는 것이 최선이 아닌가 싶습니다. Covid-19 관련하여 2년 가량 중단되었던 BOXIM workshop 공개강좌가 2022년 6월부터 다시 열립니다. 삼성서울병원 인턴/전공의/fellow 뿐 아니라 타병원 인턴/전공의/fellow/군의관/봉직의 등 누구나 참석할 수 있습니다 (유료). 여러분의 많은 관심과 참여를 부탁드립니다. (담당자)
우리나라에서 1년에 얼마나 많은 위내시경이 시행되고 있을까요? 최근 기사를 소개합니다.
[2018-5-4. 메디파나 뉴스] 내시경 검사 급증… 내시경실 적정성평가 진행된다
지난해 요양급여비용 청구건을 보면, 상부소화기내시경은 약 344만건, 대장내시경은 약 211만건에 달했다.
국민건강보험공단 건강검진 통계연보에 따르면, 위내시경은 2013년 472만 9,407명에서 2016년 604만 8,812명으로 27.9% 증가했다. 대장내시경도 2013년 10만 3,547명에서 2016년 11만 7,143명으로 13.1% 증가했다.
이에 따르면 요양급여청구 위내시경이 344만 (2017년), 공단검진 위내시경이 604만 (2016년) 정도 시행되는 모양입니다. 이는 모든 검사 비용을 본인이 부담하기 때문에 요양급여가 청구되지 않는 대형병원 검진센터의 위내시경은 포함되지 않은 숫자입니다. 그렇다면 우리나라에서 1년에 위내시경이 1,000만 건 정도 시행되는 셈입니다. 놀랍지 않습니까? 매년 1,000만건의 위내시경 검사가 시행되는 나라에 제대로 된 내시경 training center가 하나도 없다니 더욱 놀랍지 않습니까?
적절성 평가가 내시경 검사의 품질을 높일 것이라고 생각하는 분들이 많습니다. 그럴 수도 있습니다. 그러나 적절성 평가는 최소 수준의 기준을 제시하는 것일 뿐, 여차하면 하향평준화를 가져올 위험도 있습니다. 충분한 투자와 제대로 된 training이 함께 추진되어야 합니다.
오늘은 휴일이었지만, 집에 어린이가 없는 관계로 병원에서 6명의 초심자를 대상으로 endoscopy box simulator training 개인 교습을 하였습니다 (내시경 교육에는 왕도가 있습니다. 개인교습입니다). 내과 전공의 3명, 내과 전문의 1명, 외과 전공의 1명, 외과 전문의 1명이었습니다. 힘들었지만 보람된 시간이었습니다. 제대로 된 내시경 training center를 만들어 보고자 합니다.
 4. 내시경 검사 건수 - 많은 검사를 해야 하면 내시경 검사의 품질을 유지할 수 없습니다. 1시간에 5명이 maximum입니다.
4. 내시경 검사 건수 - 많은 검사를 해야 하면 내시경 검사의 품질을 유지할 수 없습니다. 1시간에 5명이 maximum입니다.
[2019-1-5 데일리 메디] 내시경 안전지표 → 시행 건수 대비 '전문인력’
내시경 지표로 인력과 검사 건수라는 개념이 처음으로 제시되었습니다 ([2019-1-5 데일리 메디] 내시경 안전지표 → 시행 건수 대비 '전문인력’). 매우 중요한 변화이므로 기사의 전문을 옮깁니다.
내시경 검사실마다 의사와 간호사는 1인 이상 상주해야 하며 시간이 오래 걸리는 치료내시경의 경우에는 간호인력 2인 이상의 기준이 있어야 한다는 분석이 나왔다. 내시경실 안전관리를 위한 기본적 지표다. 최근 건강보험심사평가원은 대한소화기내시경연구재단에 ‘내시경실 환자안전 관리방안 및 평가기준 개발’ 연구를 의뢰했고 현재 관련 내용을 검토 중이다.
이 연구가 진행된 이유는 많은 의료기관에서 검사실, 의료인력에 비해 과도하게 많은 내시경검사를 시행하고 있다는 문제가 발생하고 있기 때문이다. 물론 낮은 내시경 수가에 기인한 바 크지만 이로 인해 오진율과 합병증 발생이 필연적으로 증가하고 있는 추세다. 연구재단은 “검사실, 인력 대비 적절한 내시경 검사의 건수는 안전한 환경을 위한 기본적인 지표다. 많은 검사를 하기 위해서는 검사실, 장비의 확충과 인력 보강이 반드시 필요하다”고 진단했다. 이를 위해 검사실마다 의사와 간호사는 1명 이상 상주해야 하며 복잡하거나 시간이 오래 걸리는 치료내시경을 하는 동안에는 간호인력이 2명 이상이 근무해야 한다는 결론을 내렸다. 실제로 내시경실 및 회복실 전체 간호인력, 내시경실 간호조무사 및 보조인력, 회복실 간호사 및 보조인력은 합병증 발생 감소에 유의한 영향을 미치는 것으로 확인됐다.
"회복실은 간호사 1명당 환자 10명정도 기준"
회복실 전체 간호인력 1명이 늘어날수록 치료 결장경 1만건 당 합병증은 0.131건 감소한 것으로 조사됐다. 즉, 치료내시경 1만건 당 합병증 1건을 줄이기 위해서는 회복실 전체 간호인력이 약 8명 늘어나야 한다는 것이다.(1/0.131=7.63) 흥미롭게도 내시경 검사실 갯수 및 넓이가 증가할수록 합병증 발생 역시 증가하는 것으로 도출됐다. 이는 내시경실 크기가 큰 기관에서 난이도 높은 치료내시경 시술이 실시됐을 가능성을 예측하는 지표로 해석된다. 연구재단은 “회복실 인력 기준은 현재 50%이상 상급종합병원에서 간호사 1명당 10명 이상의 환자를 돌보는 것이 현실이므로 향후 의원급이나 병원급에서도 상향된 기준의 적절한 간호인력 확충이 필요하다”고 분석했다. 특히 “안전한 내시경실 환경을 구축하기 위해서는 안전사고와 합병증의 발생을 분석하고 재발을 방지하는 것이 중요하다. 이를 위해 지속적인 평가와 적절한 수가의 산정은 필수적”이라고 덧붙였다.
핵심 내용을 빙빙 돌려서 설명하고 있으므로 정확한 point를 잡기 어렵습니다. 그러나 요점은 다음과 같다고 생각됩니다. 한 명의 의사가 너무 많은 검사를 하면 안 된다. 내시경 검사실에 한 명의 의사가 상주하라는 말은 양방으로 검사하면 안된다는 것과 같은 말입니다. 걱정되는 분들 많으시죠?
"한 명의 내시경 의사가 한 시간에 몇 건의 검사를 하는가?" 이것이 가장 핵심 지표라고 생각합니다. 좋은 말이기는 한데요... 이를 정부에서 받아들이면 큰일입니다. 수가를 올리지 않고 검사 건수만 제한하면 그 결과는 뻔하니까요.
의료는 진지해야 합니다. 공자님도 질병은 진지하게 받아들이셨습니다. 의료는 가볍게 볼 일이 아닙니다. 늘 진지하게 접근해야 합니다. 의사는 검사를 천천히 하고 (위내시경 1시간에 5개), 정부는 적절한 비용을 지급해야 합니다.
子之所愼齊戰疾 - 論語 述而篇 13.
[대장내시경 품질과 검사 건수]
많은 검사를 해야 한다 위내시경 검사의 품질을 유지할 수 없습니다. 이는 대장내시경에서도 마찬가지입니다. 일전에 대장내시경의 새로운 질지표 (1시간에 대장내시경 2명 이하)가 제시된 바 있습니다. 수가 인상 없이는 불가능한 일인지라 잠시 이야기되다가 금방 논의가 중단되었습니다. 안타깝습니다. 우리나라에서 질 높은 내시경 검사를 할 수 없는 가장 큰 이유는 저수가입니다. 싸구려 의료 물러나라!
제가 '빠른 내시경보다 바른 내시경'을 주장하는 것은 아무리 조심스럽게 검사하더라도 속도가 빠르면 고품질 내시경은 불가능하다고 생각하기 때문입니다. 한 명의 의사가 하루에 할 수 있는 검사 숫자를 통제하는 것이 모든 질관리의 시작입니다. 위내시경은 1 시간에 5명, 대장내시경은 1시간에 2명 정도가 maximum이라고 생각합니다.
최근 대장내시경 검사의 새로운 질지표가 제시되었습니다 (심평원-장연구학회, 대장내시경 30분 이상 등 '지표' 개발 2018-1-25. 데일리메디). 저의 평소 주장과 완벽히 일치하는 개념입니다만 과연 우리나라 의료 현실에서 적용이 가능할지 의문입니다. 그러나 우리나라 정책 당국에서 의사의 검사 숫자를 제한하는 방향의 연구를 지원하고 있다는 점이 중요할 것 같습니다. 향후의 정책 방향을 짐작케하기 때문입니다.
너무 중요한 기사이므로 전문을 옮깁니다.
심평원-장연구학회, 대장내시경 30분 이상 등 '지표' 개발 2018-1-25. 데일리메디
우리나라 대장암 발병률은 세계 최고 수준이다. 세계보건기구(WHO) 산하 국제암연구소에 따르면 국내 대장암 발병률은 인구 10만명당 45명으로 조사 대상 184개국 중 가장 높다. 이러한 상황 속 대장종양절제와 관련 적정성평가가 준비되고 있다. 주목할 부분은 내시경 시간을 기준으로 한 지표가 발굴됐다는 점이다. 최근 건강보험심사평가원은 대한장연구학회에 의뢰해 대장종양절제 평가지표 연구를 마무리 짓고 관련 내용을 검토 중이다. 쟁점은 ‘일반 진단 대장내시경 30분 이상’, ‘분변잠혈검사 양성 후 대장내시경 45분 이상’이라는 지표다.
이는 대장내시경은 삽입, 회수 및 폴립절제를 위해 할당된 시간이 필요하기 때문이다. 1일 대장내시경 건수가 많아질수록 시행 의사의 피로도가 증가해 대장내시경의 전반적인 질에 부정적인 영향을 미치는 것으로 알려져 있다. 장연구학회는 적절한 의사 1인당 1일 평균 대장내시경 건수 평가지표 개발을 위해 국내 11개 대학병원에서 전향적으로 시행한 1172명의 대장내시경 자료를 분석했다. 폴립이 없는 552건의 대장내시경 평균 검사시간은 15.9분이었고, 폴립이 있는 620건의 평균 검사시간은 22.1분이었다. 분변잠혈검사 양성으로 대장내시경을 시행한 28명에서 평균 검사시간은 19.5분이었다.
학회는 “전 처치 및 준비시간을 고려할 때, 국내에서도 유럽 기준과 유사하게 적용할 필요가 있으므로 30분, 45분 기준을 준용할 필요가 있다. 환자 진료의 질을 향상시키고 다양한 시각에서 환자를 고려하는 기회가 증가하는 등 긍정적 영향을 미칠 것”이라고 밝혔다. 다만 응급 대장내시경, 계획된 폴립절제술, 수술 전 위치 확인을 위한 검사, 대장절제술 후 추적검사는 제외하기로 했다.
이를 학회 소속 19명의 전문가들에게 의견을 구한 결과, 36.8%만 동의한다는 입장이 나왔다. 평가 시 필요한 부분이긴 하지만 지표 도입 시 다소 부담스러운 부분이라는 해석으로 풀이된다. 반면 ‘기관당 전문의 1인 확보’ 94.7%, 내시경 장비 보유 ‘100%’, 보조인력 1인 보유 ‘100%’ 등 기타 구조 지표에서는 대체적으로 합의 수준이 높았다. 추후 평가 진행 시 우선 도입할 항목이 될 것으로 관측된다. 평가지표 개발과 관련, 심평원 관계자는 “대장종양절제술 평가의 필요성이 강조되고 있는 상황이고 그 첫 단계로 지표개발이 이뤄졌다. 하지만 올해 당장 추진하기는 어렵고 추후 여러 검토와 논의를 통해 평가 신설 등 결정이 이뤄질 것”이라고 밝혔다.
 6. Missing rate for gastric cancer
6. Missing rate for gastric cancer
위내시경에서 위암을 놓치는 경우는 어느 정도일까요?
위암 miss rate를 평가하는 연구방법이 모두 달라서 하나의 답을 내기는 어렵습니다. 2016년 이 주제에 대한 메타분석을 참고하는 것이 좋겠습니다. 약 10%라고 합니다. 위암 10개 중 하나는 놓친다고 생각하는 것이 합리적일 것 같습니다 (Eur J Gastroenterol Hepatol 2016). 겸손하고 또 겸손할 수 밖에...
Results: The studies included (n=22) were grouped by study design. The pooled negative predictive value was 99.7% (95% confidence interval 99.6-99.9%). Missed GCs proportion was 9.4% (95% confidence interval 5.7-13.1%), being 10.0% in studies including patients with negative EGD followed over time, 8.3% in studies including patients with GC, and 23.3% in studies evaluating the proportion of missed synchronous lesions. Mainly, missed cancers were located in the gastric body both in Eastern and in Western studies (39 and 47%, respectively). The majority of missed GCs were adenocarcinomas. Younger age (<55 years), female sex, marked gastric atrophy, gastric adenoma or ulcer, and inadequate number of biopsy fragments were reported as predictive factors for diagnostic failure.
Conclusion: EGD is a very effective method to rule out GC. However, missing GC with EGD is not uncommon, with one out of 10 cancers being potentially missed. Interestingly, lesions were more often missed in the body and therefore a more rigorous protocol for endoscopy and biopsy should be implemented worldwide.
[위게실]
참고문헌을 찾을 수 없습니다만, 위게실의 발견율을 위내시경 검사의 질지표로 사용할 수 있다는 논문을 본 적이 있습니다. 위게실 자체가 무슨 중요한 의미가 있는 것은 아니지만 위게실을 잘 발견할 정도로 구석까지 정성껏 살폈다면 훌륭한 검사라는 의미일 것입니다.
50대 남성입니다. 위게실을 발견하였습니다.
그런데 환자가 6개월 전 내시경 검사를 받았다고 하더군요. 그래서 과거 사진을 살펴보았습니다.
전정부가 첫 사진이라 정확히 검사 시간을 측정할 수 없었지만, 첫 사진은 10시 20분 1초이고 마지막 사진은 10시 20분 46초였습니다. 대부분 사진이 흔들리거나 흐린 상태였는데 contrast enhancement는 A1으로 되어 있었습니다. 너무하였다는 생각입니다.
빠른 내시경보다 바른 내시경을 합시다. 상부내시경 검사의 최소 검사 시간은 5분입니다.
2014년 환자입니다. 그때까지만 해도 내시경을 빨리 하는 의사들이 많았습니다. 그러나 현재는 '위내시경 검사 시간은 최소한 5분'이 거의 standard가 되었습니다. (저만의 착각일까요?)
내시경 검사 시간이 짧았던 시절에는 안타까운 사연이 많았습니다. 2013년 환자인데 50대 남성이셨습니다. 보만 4형 진행성 위암이고 이미 복수까지 발생된 상황이었고 palliative chemotherapy밖에 할 수 없었습니다. 그런데, 환자는 8개월 전에 내시경 검사를 받으셨다고 하셨습니다. 그 때 사진을 살펴보니... 아뿔사... 위내시경 검사 시간이 2분도 되지 않았습니다. 사진은 23장 있었지만 위체하부의 주름이 잘 나오도록 공기를 충분히 넣은 상태의 사진은 없었습니다. 그나마 위 주름이 찍힌 몇 장의 사진을 후향적으로 살펴보았는데... 정상은 아니었습니다. 경험많은 의사가 천천히 검사하였다면 충분히 진단할 수 있는 상황이었다고 추정되었습니다.
그렇습니다. 2분짜리 검사라면... 그 많은 질지표가 다 소용없는 일입니다. 사진 많이 찍는다고 검사 잘 한 것 아닙니다. 천천히 자세히 보는 것이 좋은 검사입니다. '위내시경 검사는 최소한 5분'이라는 이 단순한 원칙을 꼭 지키도록 합시다.
요약합니다. 빠른 검사는 후진 검사입니다. '빠른 내시경보다 바른 내시경'을 위해 노력합시다.
[More cases]
십이지장 33:33, 위암 발견 34:06, 조직검사 34:48, 상부식도 35:26. 2분도 안되는 내시경 동안 위암도 발견하고 조직검사를 했으니 감탄이라도 해야 하는 것일까요?
[2019-8-17. 속편한내과 심포지엄 참석자 질문]
최근 내시경에서 miss 되었던 진행성 위암 환자 증례가 시사하는 바 크다고 생각합니다.
현실적으로 상부위장관 증세로 내원한 환자가 불과 얼마 전에 타의료기관에서 내시경 검사를 받았고 별 이상이 없다고 들었으면 재검을 할 수도 없고 안 할 수도 없는 상황이 됩니다. 선생님은 어떤 기준으로 재검 여부를 결정하십니까?
[2019-8-17. 이준행 답변]
매우 어려운 질문입니다. 한 마디로 '검사 시간'입니다.
위암을 놓치지 않기 위해서 내시경 의사의 실력과 충분한 검사 시간이 중요합니다. 실력없는 의사는 병을 보고도 진단하지 못할 수 있습니다. 충분한 training과 많은 임상경험이 중요합니다. 여기까지는 너무 당연한 이야기입니다.
문제는 '어느 정도가 충분한 검사 시간인가?'입니다. 아래 서울성모병원의 자료를 보더라도 관찰시간 4분 (연구에서는 십이지장으로부터 나오는 시간만 계산하여 3분을 기분으로 나누었습니다만, 들어가는 시간을 고려하면 실제로는 4분이 기준점입니다) 미만에서는 종양성 질환의 진단율이 엄청 떨어집니다.
유럽에서는 위내시경 검사시간 7분을 중요한 질지표로 제시하고 있습니다.
저는 우리나라 환경에서 위내시경 검사시간은 최소한 5분은 되어야 한다고 주장하고 있습니다. 아래 동영상을 보시기 바랍니다. Box simulator로 (1) 공기를 넣지도 않고, (2) 침을 suction하지 않고, (3) 사진도 찍지 않고, (4) 두리번 거리지 않고 그냥 식도와 위에 들어갔다 나오는데 1분 20초가 걸렸습니다. 공기도 넣고 침도 suction하고 사진도 찍으면서 두리번 두리번 골고루 십이지장까지 살피려면 최소한 5분은 필요합니다.
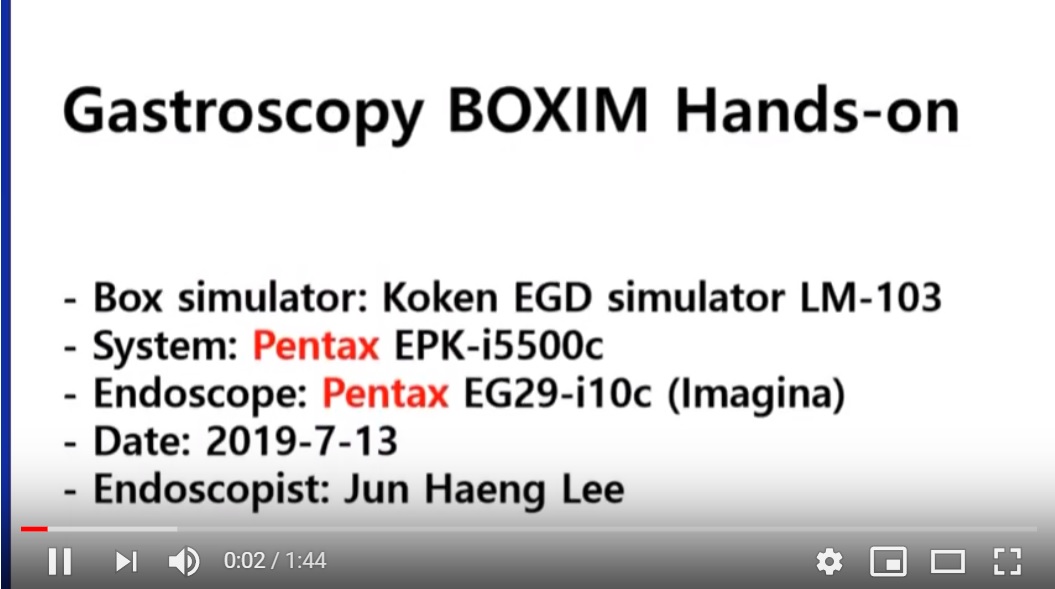
Pentax endoscope + new simulator
어떤 선생님께서는 "전 병원에서 누가 검사를 했는가를 보고 판단한다"라고 말씀하셨는데 어느 정도 타당성은 있습니다. 그러나 누가 내시경을 했는지 알기 어려운 경우도 많을 뿐더러, 설혹 경험이 많은 사람이 검사를 했더라도 질병을 놓치지 말라는 법이 없습니다. 저는 내시경 의사의 실력 못지 않게 내시경 검사 시간을 중요하게 생각합니다. Screening setting에서는 검사 시간이 더 중요합니다. 전 병원의 내시경 검사 시간이 4-5분도 되지 않으면 재검을 권하는 경우가 많습니다. 아무리 경험 많은 의사가 검사했더라도 검사 시간이 짧다면 좋은 검사를 받았다고 말하기 어렵습니다.
사진의 많고 적음은 내시경 검사의 질과 아무런 상관이 없습니다. 아래 환자는 위암이 두개였는데 위체하부 전벽의 암은 첫 관찰(노란색 box)에서 발견되지 않았다가 위체중상부 암을 발견한 이후에 공기를 많이 넣고 검사하는 과정에서 뒤늦게 발견되었습니다.
오늘 식사 중 어떤 선생님께서 이런 말씀을 하셨습니다. "차라리 과거 폴라로이드로 사진 4장 찍었을 때 더 자세히 관찰했던 것 같다. 많은 사진을 찍는 것 자체가 검사에 방해가 될 수 있다." 전적으로 동의합니다. 위내시경이나 대장내시경이나 사진 15장이면 충분합니다. 그 이상은 noise입니다. 자세히 보는 것이 중요하지 사진의 수가 중요하지 않습니다.
진정(수면)내시경도 검사의 정확도가 낮을 수 있습니다. Procedural sedation 수준-환자가 잠자지 않을 정도-으로 아주 약하게 sedation을 하면서 검사하는 것이 원칙입니다. 이렇게 하면 진단의 정확도에는 아무런 문제가 없습니다. 그런데 우리나라에서는 서구에서 권하는 용량보다 2배 이상 많은 약을 사용하여 푹 재우는 경우가 많습니다. 그 과정에서 paradoxical response도 많고, 환자의 협조가 잘 되지 않아 충분히 검사하지 못하는 예가 적지 않은 것 같습니다. Propofol을 쓰면 검사 도중 환자가 깨는 경우가 있어서 더 보고 싶어도 그냥 나오는 경우도 있다고 들었습니다.
검사 시간이 아주 짧은 검사는 대부분 진정(수면)내시경이었던 것 같습니다. 맨정신으로 검사를 하면서 검사시간이 아주 짧으면 환자로부터 "제대로 본 것이냐?" 항의받기 마련이므로 조금 천천히 자세히 보지 않을 수 없습니다. 물론 협조가 안 되어 검사 자체가 어려운 경우도 있지만... 여하튼 수면이냐 아니냐는 중요하지 않습니다. 잘 보는 것이 중요합니다. 잘 보는 것의 가장 중요한 조건은 길게 보는 것입니다. 오래 봐야 암을 놓치지 않습니다. 최소한 5분입니다. 평균 검사 시간이 5분은 되어야 정상입니다.
한마디로 요약합니다. 저는 짧게 검사받고 오신 분은 검사 안 하신 것으로 치고 재검을 권하고 있습니다. 빠른 내시경보다 바른 내시경을 합시다.
[2020-4-8] 내시경 검사료
우연히 내시경 검사 가격표를 보았습니다. 이 가격으로 질관리를 하라니 입이 다물어지지 않습니다. 그러나 하지 않을 수도 없습니다. 검사에도 적절한 가격이 필요합니다.
[2020-12-15] 내시경학회 질관리 위원회 on-line 공청회
내시경학회 질관리 위원회 on-line 공청회에서 screenshot입니다. 통합 4주기 국가암검진 내시경 결과지에 '위내시경 시술시간' 추가를 고려해야 한다는 제안입니다. 정말 획기적인 아이디어라고 생각합니다. 100번 1000번 찬성합니다. 내시경이 입에 들어가는 순간부터 입에서 나올 때까지 최소한 5분은 필요합니다. 그게 minimum입니다.
질지표가 많다고 질이 좋아지는 것은 아닙니다. 질지표는 질이 좋아지는 방향으로 만들어져야 합니다. 지표를 잘 못 만들면 질지표만 좋아지고 실제적인 질(質)은 나빠집니다. 내시경 질지표로 가장 중요한 두 가지는 (1) 내시경 시술 시간, (2) 시술자의 교육/훈련이라고 생각합니다. 딱 하나만 들라면 '내시경 시술 시간'입니다. 위내시경 검사 시간은 최소한 5분은 되어야 합니다. 그게 질입니다.
우리나라에서 내시경을 제대로 배우려면 소화기내과 fellow 과정은 필수입니다. 대충 배워 아주 초보적인 screening을 하려고 해도 3개월 full time training이 필요합니다. Dedicated center에서 열성적인 선생에게 3개월은 배워야 가장 기초적인 위내시경을 할 수 있습니다.
[2021-1-24] 내시경학회-소화기학회 경인지회 합동 연수강좌
상부내시경 관련 강의를 잘 들었습니다. 나름대로 요약하였습니다. (만년필 동호회 style로 촬영)
[2021-3-30] fast hand?
얼마 전 어떤 질문을 받고 어이가 없어서 5분 검사시간을 강조하는 답변을 했습니다.
배울 때부터 제대로 배우고, 바르게 내시경 할 수 있는 제대로 된 환경을 만들고, 제대로 하고 있는지 monitoring 하는 것... 이 모든 것이 필요합니다. 안타깝습니다. 저수가 환경이 지겹습니다.
[2021-7-7. 애독자 편지]
이준행 교수님 안녕하십니까?
전임의 시절부터 오프라인 강의와 엔도투데이 잘 살펴보고 있는 소화기내과 의사입니다. 다름이 아니라 양심상 답답해서 상담(?), 하소연 드려봅니다. 현재 제가 근무하고 있는 병원은 ...... 소화기내과 의사는 저 혼자이고, 다른 1명은 가정의학과 선생님, 그리고 2분의 신장내과 선생님이 계시지요. 당연히 내과 검진내시경 담당은 저와 가정의학과 선생님입니다.
내시경기계는 Olympus CV190(3대), H170 (4대)series를 쓰고 있는데... 내시경 끝의 bending이 잘 되지 않습니다. 최대로 up을 걸어도 160~170도 정도 밖에 안되고, 매뉴얼처럼 210도는 커녕 180도도 안 나옵니다. 내시경 담당 간호사분께 말을 했는데, 올림푸스에서 와서 봐줬는데 내시경이 오래 되서(낡아서) 그런거라고...속의 wire를 더 죄어줄수는 있는데, 얼마 못가서 다시 풀릴거란 소리를 들었답니다. 병원측에 말은 해 놓았는데, (당연히 Covid-19로 인하여 병원사정이 안 좋아져서) 교체나 신품구입은 힘든 상황입니다. 지금은 아직 검진 비수기라서 하루에 10명정도의 환자분을 위내시경 검사를 하는데... 앞으로 다가올 성수기때는 어찌해야할지... 최대한 up을 해도 bending이 제대로 안되니 cardia 부위를 관찰하기가 매우 힘듭니다. Stomach의 angle부분이야 어떻게든 조작해서 겨우겨우 찍고 있지만, cardia 부위는 (sample 사진을 보시면 아시겠지만) 진짜로 어떻게 시도를 해보아도 잘 안보입니다. 선생님께서는 좋은 방법이 있으신지요?
항상 선생님께서 강조하시는 대로 빠른 내시경보다는 바른 내시경을 추구하고 있는데... 양심상 답답합니다. 나는 잘 보고 싶은데, (회사택시)가 안 좋아서 잘 관찰 못하는... 2021년도에 모 유명 검진기관에 근무하였을 때에도 오전 1session에만 위내시경 50개, 60개씩(1인당 1~2분! 내시경관찰시간이 되더군요...) 하여서 바른 내시경보다는 빠른 내시경을 했었는데, 도저히 이건 아니라고 생각하여 이직한 병원이 이렇습니다... 병원측은 어디까지나 정형/신경외과가 주력이 되어 수익을 담당하고, 내과는 그저 병원 규모에 맞게 꾸며놓은 것이라서 내시경실도 많이 부족합니다. 내시경실 담당 간호사도 4명 밖에 안되고, 아무튼 뭔가 어설픕니다.
이대로 양심에 가책을 받아가면서 내시경을 해야하는것인지, 아니면 타 병원으로의 이직을 고려해야하는지...(현재도, 수도권에 있는 2차병원급 병원도 알아보고 있습니다.) 솔직히 답이 없는 문제이긴 하지만, 그래도 답답해서 하소연 드려봅니다. 앞으로도 선생님의 강의 및 endotoday 자주 찾도록 하겠습니다. 읽어주셔서 감사합니다.
[2021-7-7. 이준행 답변]
예. 누구나 고민하는 우리나라 의료의 현실입니다. 박정희 독재 때 시작된 저가 공짜 선심성 의료가 정권이 갈려도 호전되기는 커녕 점차 악화되는 상황입니다. 그에 더하여 의료 자본가들이 건진 쪽에 포진하여 국민의 피를 빨고 있습니다. 여러 후배 의사들이 편하게 일할 수 있는 여건을 만들지 못해 죄송합니다. 이준행
[2023-9-23. KSGE webinar review]
[2024-9-25] 내시경 가격 중 "암(중증)환자 이며 암 산정특례 자격이 있는 환자의 경우, 검사료 급여 5% 부담, 진정내시경 검사관리료 급여 5% 부담" 조건에서 환자가 부담하는 비용은 아래와 같습니다. 좋아해야 할지 어떻게 반응해야 할지 당황스러울 뿐입니다.
[2025-7-26]
[2025-11-20] GLP-1 투약 환자에서 내시경 실패률이 높습니다.
3) EndoTODAY Colonoscopy withdrawal time - 6 minutes issue
4) EndoTODAY 내시경 속도 - 빠른 내시경보다 바른 내시경.
5) [2018-5-4. 메디파나 뉴스] 내시경 검사 급증… 내시경실 적정성평가 진행된다
지난해 요양급여비용 청구건을 보면, 상부소화기내시경은 약 344만건, 대장내시경은 약 211만건에 달했다.
국민건강보험공단 건강검진 통계연보에 따르면, 위내시경은 2013년 472만 9,407명에서 2016년 604만 8,812명으로 27.9% 증가했다. 대장내시경도 2013년 10만 3,547명에서 2016년 11만 7,143명으로 13.1% 증가했다.
6) [2018-5-31. 데일리메디] 내년 1월 강화된 'CT·MRI 품질관리기준' 적용 - (이준행 註) 영상의학과 영역의 image quality에 대한 관심이 높아지고 있습니다. 곧 내시경 image quality에 대해서도 눈길이 가겠지요. 후진 내시경은 빨리 폐기해야 할 날이 올 것 같습니다.
7) 어떤 Facebook posting (2021-11)
8) Post-Endoscopy Upper Gastrointestinal Cancers Gastroenterology 2022;162:1123-1135.
9) [2023-5-8. 한국경제TV] 위내시경 받았는데 위암?…"의사가 3분 이상 관찰해야"
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.