 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [위용종. Gastric polyps] - 終
[위용종. Gastric polyps] - 終
1. Definition
4. Inflammatory fibrinoid polyp 염증성 섬유양 용종
5. Gastric hamartomatous polyps in polyposis and non-polyposis
6. Fundic gland polyp in PPI users
7. Other polyps
8. Adenoma/carcinoma arising from hyperplastic polyp 등
10. FAQ - NGS을 이용한 polyposis panel
11. References
용종은 내강을 향하여 돌출된 병변을 총칭하지만 흔히 좁은 의미로 사용하여 양성 상피성 종양만을 의미합니다. 간혹 metaplastic gastritis에서 보이는 납작하고 약간 융기된 metaplastic nodule을 용종이라고 부르는 경우가 있는데 이는 바람직하지 않습니다. 재검에서 보일 수도 있고 보이지 않을 수도 있는 경미한 소견을 용종이라고 부르지 맙시다.
용종의 분류는 전통적으로 Yamada 분류법이 이용되었습니다. 융기의 기시부가 둔각이고 완만하면 Yamada-I형, 융기의 기시부가 예각으로 경계가 완만하지만 잘룩하지 않으면 Yamada-II형, 융기의 기시부가 잘룩하지만 목(neck)이 없으면 Yamada-III형, 유경성(pedunculated)이면 Yamada- IV형으로 분류됩니다.
최근에는 sessile, semi-pedunculated, pedunculated 로 나누고 있습니다.
조직학적으로는 선종성 용종(adenomatous polyp)과 비선종성 용종으로 나누지만, 보통 용종이라고 하면 비선종성 용종을 말합니다. 과거에는 과형성 용종이 가장 흔했는데 최근에는 위저선용종(fundic gland polyp)이 가장 흔한 것 같습니다.
용종증 (polyposis)의 정의는 명확하지 않습니다. 한 장기에 다수의 용종이 있을 때 용종증이라고 부를 수 있으나 몇 개 이상이라는 기준은 없습니다. 10-20개 이상에서 용종증이라고 부르는 경향입니다. 아래는 이선영 교수님께서 정리한 내용입니다.
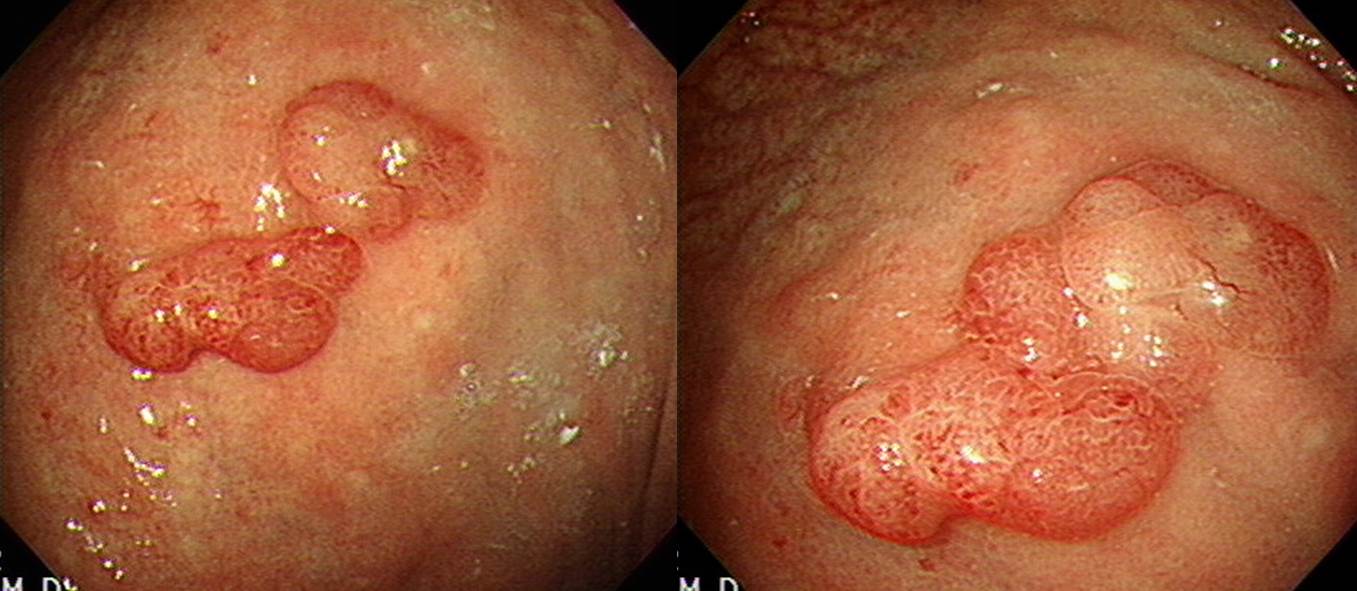
2024-24. Hyperplastic polyp
과형성 용종은 위점막 상피가 과도하게 증식한 결과입니다.
여러개의 과형성 용종이 동시에 발생하는 경향이고 2 cm이하가 많고 붉은 색깔을 띠며 작을 때는 sessile하지만 커지면 유경성이 됩니다. 암으로 진행하는 경우는 거의 없습니다. 과형성 용종은 작으면 치료가 필요없습니다.
조직학적 특징은 아래와 같이 요약됩니다. pathologyoutlines.com
서구 가이드라인은 2 cm 이상에서 내시경 절제를 하도록 권하고 있습니다. 우리나라에서는 이보다 작아도 치료를 권하는 의사가 많습니다. 치료 후 다른 곳에서 재발하는 예가 많으므로 사전에 잘 설명해야 합니다.
2년 동안 크기가 증가하였던 과형성 용종
전정부에 2개, cardia에 1개. 다발성 과형성 용종
매우 큰 Yamada type III 과형성용종
Yamada type IV 과형성용종
가지가 뚜렷하였고 가지 끝에 감이 열린 형상의 과형성 용종. 절제술 직후 출혈이 있어 지혈술을 하였습니다.
Helicobacter-associated hyperplastic polyp
과형성 용종이 transient 하게 pyloric ring을 통하여 십이지장으로 herniation 되어 있었습니다. 흡입하여 당긴 후 시술하였습니다.
용종이 어느 정도 이상 크면 절제술을 권합니다. 이유 중 하나는 출혈할 수 있기 때문입니다. 아래는 melena로 내원한 환자입니다. 용종에서 출혈한 경우였습니다. 용종절제술로 치료하였습니다.
과형성 용종 환자가 헬리코박터 감염증이 있으면 이를 치료하기도 합니다. 용종이 작아진다는 설이 있기 때문입니다. 그런데 저는 이를 잘 믿지 않습니다. 간혹 저절로 작아지는 사람도 있기 때문입니다. 아래 환자는 헬리코박터 음성이었고 특별한 치료를 하지 않았는데 추적 내시경에서 저절로 용종이 작아진 예입니다.
특별한 치료 없이 저절로 작아진 과형성 용종
조직소견이 전형적이 과형성 용종과는 달라서 병리결과가 hypertrophic gastric mucosa로만 보고되는 경우도 있습니다.
과형성 용종이 저절로 떨어지는 수가 있습니다. 완전히 없어지는 수도 있고 일부가 남는 수도 있습니다. Autoamputation이라고 부릅니다.
매우 큰 용종으로 의뢰되어 내시경절제술을 하려고 하였으나 이미 저절로 용종의 대부분이 사라진 상태였습니다.
Fundus 주변의 넓은 area가 hyperplatic change를 보이고 일부 용종이 있었습니다. 조직검사로 hyperplastic polyp으로 확인하였습니다. 특별한 치료 없이 경과관찰 하였는데 1년 후 국소적으로 튀어나와 있던 용종은 사라진 모양입니다. 저절로 떨어졌을 수도 있고 조직검사 한 부위와 가까워 떨어졌을 수도 있을 것 같습니다.
Autoamputation되면서 출혈이 발생할 수 있습니다. 그러나 이를 증명하기는 쉽지 않을 것입니다. 지금까지 문헌에 보고된 것은 단 한번뿐이라고 생각됩니다 (Nakajima T. Endoscopy 2003;35(12):1069-1071). 출혈환자에서 내시경을 해 보았더니 용종이 떨어져있고 그 자리에서 출혈한 흔적이 있었다는 것입니다. 억세게 운이 좋지 않으면 증명하기 어렵습니다.
아래 환자도 용종 하나(전정부 소만에서 전벽쪽의 가장 큰 것)가 저절로 없어진 경우입니다. Peduculated polyp은 저절로 없어질 수 있습니다.
과형성용종의 조직검사 후 출혈이 발생할 수 있습니다. Hypervascular하므로. 조직검사 후 출혈이 많으면 즉시 EMR polypectomy를 시도할 수 있습니다.
[Inverted hyperplatic polyp]
An inverted hyperplastic polyp (IHP) is a rare type of benign polyp, found in the stomach or colon, that grows downward into the submucosa instead of toward the lumen. Because of this unusual growth pattern, it can be mistaken for a subepithelial tumor or even a malignant tumor. IHPs are typically treated with endoscopic removal, and while they are benign, they can sometimes coexist with adenocarcinoma. (Google AI. 2025-11-1)
수 년 전 가톨릭의대에서 보고한 증례가 있었습니다. (Korean J Helicobacter Up Gastrointest Res 2023)
[과형성 용종 + 넓은 과형성 용종 유사 점막변화]
들문 직하부에 몇 개의 용종이 있어 들문을 감싸고 있는 양상입니다. 위체부 소만의 점막이 넓은 부위에 걸쳐 약간 두껍고 발적되어 있습니다. 급접하여 관찰하면 발적부 표면은 과형성용종의 표면과 동일해 보입니다. 과거부터 수차례 조직검사를 하였으나 항상 모두 hyperplastic polyp이었습니다. Helicobacter pylori 음성입니다. 정확한 원인을 알기 어렵습니다. 경과관찰 중입니다.
 4. Inflammatory fibrinoid polyp (IFP) 염증성 섬유양 용종
4. Inflammatory fibrinoid polyp (IFP) 염증성 섬유양 용종
Inflammatory fibrinoid polyp (IFP) 염증성 섬유양 용종은 양성 종양입니다. 악성화 보고는 보지 못했습니다. 따라서 내시경 절제술이나 수술이 꼭 필요한지 명확하지 않습니다. 내시경 절제술은 쉽지 않습니다. 뚜렷한 융기형이고 위벽에 깊게 침투하지 않은 IFP는 일반 EMR과 혹은 ESD와 비슷하게 절제할 수 있습니다. 위벽에 깊게 침투한 IFP는 내시경 치료가 쉽지 않을 수 있으므로 복강경 쐐기 절제술이 필요할 수 있습니다. IFP 염증성 섬유양 용종이라는 이름이 시사하는 바와 같이 섬유화가 심한 종양이므로 제법 단단하여 내시경 절제술 후 수거하기가 어려울 수 있습니다. 이 모든 점을 고려하여 IFP로 추정되는 용종을 치료하지 않고 경과관찰 하는 것도 가능하다고 생각합니다. 사실 암인 용종 (EGC type 1)이나, 전암성 병소인 용종 (선종성 용종) 혹은 출혈과 같은 합병증을 동반한 용종이나 점막하종양은 치료가 필요하지만 그렇지 않은 용종이나 점막하종양은 위험을 무릅쓰고 치료하기보다는 정기적인 관찰이 환자에게 더 유리한 경우도 있습니다. 저는 IFP으로 추정되는 환자에서 치료가 쉬운 병소는 내시경 절제술을 하기도 하지만 깊게 박힌 IFP에 대하여 내시경 절제술을 무리하여 시행하는 것은 그다지 바람직하지 않다고 생각하고 있습니다. (2024년 2월)
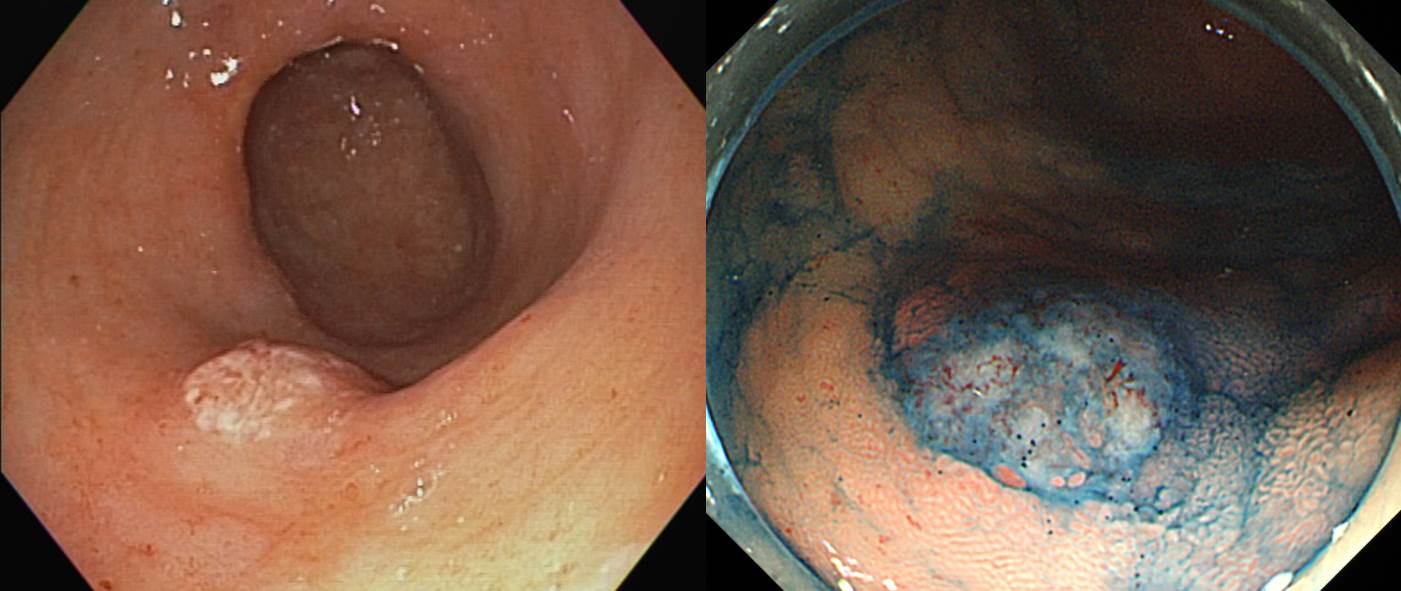
전형적인 증례 1 - EndoTODAY quiz로 출제하였습니다. 한 fellow 선생님께서 "정상적인 tubule 구조가 전혀 없고 염증 세포들, 특히 eosinophil들이 많이 보입니다. 중앙에 혈관이 보이는데 그 주변으로 fibrinoid 침착이 보입니다. 진단은 inflammatory fibroid polyp 인 것 같습니다."라는 답을 주셨습니다. Excellent!
전형적인 증례 2
Inflammatory fibrinoid polyp은 gastric submucosal granuloma with eosinophilic infiltration, eosinophilic granuloma, hemangiopericytoma, fibroma, inflammatory pseudotumor 등 다양한 이름으로 불렸던 종양입니다. 조직학적으로 섬유조직, 혈관, 호산구를 포함한 많은 염증세포들로 구성되어 있고 국소적인 비신생성 성장을 하는 질환입니다.
병리 소견은 아래와 같습니다 (pathology-on-line).
주로 위에 발생하지만 드물게 소장, 대장, 식도에서도 발생할 수 있습니다. 악성변화는 보고된 바 없습니다. 위내시경에서는 주로 pedunculated polyp의 형태가 많은데 SMT와 비슷하게 보이는 경우도 있습니다. 이 증례는 SMT처럼 보였던 경우이고 wedge resection으로 확진할 수 있었습니다. 수술전 impression은 GIST였습니다.
용종형 inflammatory fibrinoid polyp
용종형 inflammatory fibrinoid polyp
45세 남자 (2018). 점막하종양형 inflammatory fibrinoid polyp. Actin (-) S-100 (-) CD34 (+)
2016년 109회 내시경집담회에서 나수영 교수님께서 전정부 상피하 종양 양상의 inflammatory fibrinoid polyp 2예를 소개하였습니다. c-kit 음성, s-100 음성, CD34 양성이 비교적 특이한 소견이라고 합니다.
Gastric fundus에서도 발생할 수 있습니다.
원의 전정부에서 발생하여 십이지장 쪽으로 herniation을 보인 증례입니다.
십이지장에서도 발생할 수 있습니다.
 5. Gastric hamartomatous polyps in polyposis and non-polyposis
5. Gastric hamartomatous polyps in polyposis and non-polyposis
1) In polyposis
Cowden syndrome에서 hamartomatous polyposis가 발생합니다.
2) In non-polyposis
전정부 후벽, 날문에 닿아서 바닥이 넓은 결절형 용종입니다. 조직검사에서 hyperplastic polyp 소견으로 EMR을 하였고 hamartomatous polyp으로 나왔습니다.
Polyposis가 아닌 gastric hamartoma는 무척 보기 어렵습니다. 박재근 선생님께서 정리한 바를 소개합니다.
 6. Fundic gland polyp in PPI users
6. Fundic gland polyp in PPI users
PPI 사용 후 fundic gland polyp이 발생한 예는 종종 만나게 됩니다.
PPI를 끊고 fundic gland polyp의 수가 감소하였다는 증례보고도 있습니다. 발생기전에 대해서도 충실히 설명되어 있었습니다 (김진수. 대한소화기학회지 2008;51:305-308).
PPI와 관련된 fundic gland polyp의 임상적 의의는 거의 없다고 생각됩니다. 작고 한두개면 조직검사로 제거할 수도 있고 조금 더 크면 용종절제술로 쉽게 해결할 수 있습니다만 꼭 제거해야 하는지 의문입니다.
Sessile hyperplatic polyp (1 year interval)
Fundic gland polyp, sporadic. 자세히 보기
Fundic gland polyp, sporadic
GERD로 장기간 PPI standard dose를 매일 복용하고 있던 분에서 우연히 발견된 polyp. 조직검사를 하였고 그 과정에서 polyp은 제거되었습니다. 병리결과는 fundic gland polyp이었습니다. PPI user에서 fundic gland polyp이 종종 발견되지만 그 빈도는 잘 알려져 있지 않습니다. 한 가지 확실한 것은 precancerous lesion은 아니라는 것입니다. 별다른 임상적 의의가 없다고 생각해도 무방합니다.
Fundic gland polyposis in FAP. 위저선 용종은 FAP 환자의 90%에서 발견됩니다. FAP 환자가 아닌 일반인에서 우연히 발견되는 소수의 산발적 위저선 용종은 전암성 병소가 아니므로 아무런 치료도 필요하지 않습니다. 그에 반하여 FAP 환자의 위저선 용종은 40% 정도에서 이형성을 보입니다. 즉 FAP 환자의 위저선 용종은 병리학적인 관점에서 산발적인 위저선 용종과 차이가 있습니다. FAP 환자에서 위저선 용종의 이형성이 선행된 상태에서 이차적으로 APC 변이가 발생시에는 매우 드물지만 전암성 병소가 될 가능성도 가지고 있습니다. 그러나 그 빈도는 매우 낮기 때문에 FAP에서 발견되는 위저선 용종에 대해서는 특별한 치료를 하지 않고 경과관찰만을 권하고 있습니다.
FAP로 total colectomy를 받으신 분의 위내시경에서 위저부와 위체부에 다발성 용종이 발견되었습니다. 전형적인 fundic gland polyposis입니다. 조직검사에서 fundic gland polyp으로 판독되는 것이 당연하겠지만 간혹 hyperplastic polyp으로 판독되기도 합니다. 병리판독 결과와 무관하게 이런 경우는 fundic gland polyposis가 옳습니다.
Retention polyp
Retention polyp
Hamartomatous polyp
Lympoid polyp
Herniated gastric mucosa in the submucosa
Hamartomatous inverted polyp (위 증례 38)
Wedge resection: Inverted hyperplastic polyp with focal inflammatory myofibroblastic tumor-like stroma (1.3x1cm)
Hyperplastic polyp with focal high grade dysplasia
Serrated adenoma
EGC type 1
Gastritis cystica profunda (참고: ESD로 제거한 gastritis cystica profunda 2022 상부위장관학회지)
Perineurinoma (= benign fibroblastic polyp)
위용종절제술을 하려는데 환자가 괜히 췌장이 걱정된다고 CT도 함께 처방해 달라고 요청하셨습니다. 그래서 위용종절제술 후 CT를 찍었는데요... 우연히 용종절제술 자리 주변으로 작은 extraluminal air가 있었습니다. 염증 소견은 없었고, 환자에게 전화로 확인하였는데 증상도 없다고 합니다. 비단 용종절제술 뿐만 아니고 조직검사 직후에 CT를 찍어도 간혹 extraluminal air가 있다고 나오는 경우가 있습니다. 임상적 의의는 없다고 판단됩니다.
 8. Adenoma/carcinoma arising from hyperplastic polyp 등
8. Adenoma/carcinoma arising from hyperplastic polyp 등
Hyperplastic polyp으로 생각하고 위용종절제술 후 암이나 선종으로 나와 놀라는 경우가 있습니다. 1cm 이상의 hyperplastic polyp은 제거할 것을 권하고 있습니다. (2021-7-16. 이준행)
adenoma with HGD arising from hyperplastic polyp (2015)
위각부 과형성 용종으로 2년마다 추적관찰하던 중 최근 조직검사에서 adenoma가 나와 의뢰된 분입니다.
Stomach, ESD:
Tubular adenoma with high grade dysplasia in hyperplastic polyp
1. Location : angle, lesser curvature
2. Gross type : elevated
3. Size of adenoma : (1) longest diameter, 12 mm (2) vertical diameter, 11 mm
4. Resection margin : negative resection margins(N)
Stomach, upper body, greater curvature, "1", polypectomy :
Tubular adenocarcinoma, poorly differentiated , arising in hyperplastic polyp
1) size of carcinoma: 0.2x0.2 cm
2) lymphatic invasion: not identified
3) perineural invasion: not identified
4) negative resection margins (0.4 cm apart from deep resection margin)

Stomach, antrum, greater curvature, polypectomy:
Focal mucosal carcinoma (signet ring cell carcinoma) associated with globoid dysplasia;
1) size of carcinoma: up to 2 mm
2) negative margin
ESD: Early gastric carcinoma
1. Location : antrum, greater curvature
2. Gross type : EGC type IIa
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 8 mm (2) vertical diameter, 6 mm
6. Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
7. Resection margin : free from carcinoma(N), safety margin : distal 8 mm, proximal 4 mm, anterior 10 mm, posterior 12 mm, deep 500 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
조금 이상한 경우입니다. 외부 조직검사에서 W/D adenocarcinoma로 나와 의뢰된 경우로 ESD를 했는데 최종 병리결과는 hyperplatic polyp이고 암으로 된 부위는 없다고 나왔습니다. 암 진단을 없던 일로 하고 산정 특례를 취소하였습니다.
Hyperplastic polyp으로 생각하여 one stage polypectomy 후 암이 나와 의뢰되었습니다.
Stomach, polypectomy : ADENOCARCINOMA, WELL DIFFERENTIATED, arising in hyperplastic polyp;
1. Location : antrum, posterior wall
2. Gross type : EGC type IIa
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 5 mm (2) vertical diameter, 4 mm
6. Depth of invasion : invades mucosa (lamina propria, muscularis mucosa) (pT1a)
7. Resection margin : free from carcinoma(N) safety margin
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
Polypectomy pathology: tubular adenoma in the backtround of hyperplastic polyp
위용종절제술을 위하여 의뢰된 환자입니다. 다시 관찰하니 용종의 base가 pyloric ring에 위치하였는데 십이지장쪽으로 약간 치우친 느낌이었습니다. 십이지장용종으로 판단되었고 용종절제술을 하였고 Brunner gland hamartoma로 진단되었습니다.
[More duodenal polyps]
[2016-6-10. 애독자 질문]
교수님 안녕하십니까? 엔도투데이 애독자입니다.
개인의원에서 대장 용종절제술은 많이 시행되는 반면, 위 용종절제술은 개인의원에서 잘 시행하지 않고, 대부분 대학병원으로 전원하는 것으로 알고 있습니다. 그 이유를 제가 주변 지인들의 의견을 구해보고 또 생각해 본 결과로는 (1) 위가 대장보다 arterial blood supply 를 여러 곳에서 많이 받기 때문에 artery pumping 등 bleeding risk 가 더 크고, (2) 위내시경할 때는 구역질, 트럼 등을 할 경우 시술할 때 위험할 수 있고, (3) 위산이 있으므로 시술 후 iatrogenic ulcer 가 생겨 통증이 생길 수 있어서,(4) 대장용종절제술은 많이 해봤지만, 위용종절제술은 많이 해보지 않아서 막연히 겁이 나서 일 것 같은데요...... 교수님께는 두 가지 문의를 드립니다.
(1) 만약 대장용종절제술이 숙달된 의사라면, 위 용종절제술을 개인의원에서 해도 된다고 생각하시는지요?
(2) 개인의원에서 대장용종절제술은 많이 해도 위용종절제술은 잘 하지 않는 이유가 무엇인지요?
[2016-6-19. 이준행 답변]
첫번째 질문에 대한 답변은 당연히 Yes입니다. 대장용종절제술이 위용종절제술보다 어렵습니다. 대장용종절제술을 잘 하시는 분에게 위용종절제술은 쉬운 일입니다. 느낌이 조금 다르지만 한두번 해보면 금방 차이를 알게 됩니다. 따라서 두번째 질문에 대하여 답하겠습니다.
1. 위 용종은 대부분 제거할 필요가 없습니다. 작은 sessile hyperplatic polyp이 대다수입니다. 저는 보통 2 cm 정도 되었을 때 용종절제술을 권합니다. Pedunculated polyp이나 semi-pedunculated polyp의 경우는 그보다 작더라도 환자가 강력히 원하면 시술하기도 합니다 (말리는 것보다 시술 해버리는 편이 간단하니까). 그러나 sessile polyp은 여간해서는 건드리지 않습니다. 용종절제술이 필요하지도 않고 무리해서 시도하면 제법 출혈이 많습니다. 조직검사 1-2개면 족합니다.
2. 위용종절제술 전 조직검사를 하는 것이 좋습니다. 즉 한번에 못합니다. 조직검사를 하고 그 결과를 확인한 후 시술해야 하기 때문에 개업가 업무 flow로 볼 때 무척 불편한 일입니다. 반면 대장용종절제술은 한번에 끝나므로 상대적으로 간단합니다. 조직검사가 필요한 이유는 일전에 설명드린 바 있습니다. 조용해 보여도 간혹 암일 수 있기 때문입니다. 아래에 다시 옮깁니다 (출처: EndoTODAY 조직검사).
치료내시경 전에도 조직검사는 필요합니다. 조직검사를 하지 않고 바로 치료에 들어갔을 때 어떠한 결과가 나올 수 있는지를 증례를 통하여 말씀드리겠습니다. 위용종절제술 후 의뢰된 환자입니다. 전정부의 Yamada type III 용종에 대하여 용종절제술이 시행되었습니다. 사전에 조직검사가 시행되지는 않았던 것 같습니다.
그런데 용종절제술 병리결과가 예상밖으로 나왔습니다. 제 1형 조기위암이었고 multiple lateral margin positive였습니다.
완전절제가 되지 못한 상황이었고 일주일 후 추적 내시경 조직검사에서 residual cancer가 확인되어 큰 병원으로 의뢰되었습니다. 조직검사를 통한 조직진단을 하지 않고 치료를 하였을 때에는 종종 이와 같은 안타까운 결과가 발생합니다. 이 정도의 용종은 조직검사로 확인한 후 치료에 들어가는 것이 맞다고 생각합니다. 빠른 치료보다는 바른 치료가 더 중요하기 때문입니다.
만약 조직검사를 통하여 사전에 암이라는 사실을 알았더라면 어떠한 차이가 있었을까요? 이 증례는 전정부 소만의 과형성 용종을 의심하였은데 조직검사에서 분화가 좋은 위선암으로 나왔습니다.
위암 내시경치료의 일반적인 원칙을 지켜서 충분한 resection margin을 확보하며 one piece resection을 하였습니다. 최종 병리결과에서 완전절제로 확인되었습니다. 조직검사가 있었는지 없었는지에 따라서 이처럼 큰 차이가 발생할 수 있습니다. 지금까지 조직검사의 중요성에 대하여 말씀을 드렸습니다.
3. 제법 합병증이 많습니다. 출혈 말입니다. 절제술 직후 바로 지혈술을 해야 하는 경우도 있고 지연 출혈도 있습니다. 이를 예방하기 위하여 혹은 아무 것도 안 했다는 비난을 피하기 위하여 PPI 혹은 H2RA를 투여합니다 (대장에서는 투약이 필요하지 않습니다). 또 다른 측면도 있습니다. 출혈이 발생하면 환자에게 미치는 정신적 충격이 전혀 다릅니다. 피똥을 싸는 것과 피를 토하는 것은 전혀 다른 경험입니다.
4. 수가가 형편없습니다. 사실 이게 가장 중요한 이유일 수 있습니다. 아시다시피 수 년 전 대장용종절제술 수가가 상향조정되었습니다 (물론 그로 인한 부작용도 많았습니다). 위는 아닙니다. 위용종절제술은 아직 500원짜리 짜장면입니다.
[2016-6-24. 애독자 질문]
Colon 에서 pedunculated polyp 을 polypectomy 를 할 때, base까지 완전히 절제하지 말고, stalk 을 남겨 두어야, bleeding 할때, clip 으로 치료할 수 도 있으므로, stalk 을 2분의 1 또는 3분의 2 정도 남겨두라는 말씀을 어떤 교수님의 학회 강의에서 들었었습니다.
제 경험으로도 stalk 을 남겨 둔채로 polypectomy를 했을때, 병리 report 에서는 adenoma, resection margin free 로 나왔던 적이 몇번 있습니다.
Stalk 이 남아 있어도 resection margin free 인 것을 보니, stalk 은 dysplasia 가 없는 normal tissue 인지 궁금하여 문의드립니다.
[2016-7-9. 이준행 답변]
Pedunculated polyp은 처음부터 pedunculated polyp이 아닙니다. 처음은 sessile polyp으로 시작합니다. 점차 polyp이 커지면 위장관 연동운동의 영향을 받아 점차 늘어나게 됩니다. 용종 아래부분의 점막이 조금씩 늘어나 결과 peduculated polyp이 되는 것이지요. Peduculated polyp의 head 부분은 과형성용종, 선종, 암 등이지만 neck 부분은 늘어난 정상 조직입니다. 마치 혹부리 영감의 혹처럼 쭉 늘어진 결과 peduculated polyp이 되는 것입니다.
[2019-7-4. Information]
BL829002 Colorectal Cancer, Polyposis Panel 이 신설되어 공지 드립니다.
1) 적응증
- 30개 이상의 polyp이 발견되는 polyposis 환자
- Bethesda혹은 amsterdam criteria에 해당되어 유전대장암이 의심되는 환자2) 방법: candidate 유전자에 대한 NGS (next generation sequencing) 실시 - 검사 소요시간 2달
- Lynch: MLH1, MSH2, MSH6, PMS2, EPCAM,
- adenomatous polyposis AD : APC, POLE, POLD1, AR: MUTHY, NTHL1, MSH3
- Peutz-jegher SD: STK11
- Juvenile polyposis: SMAD4, BMPR1A,
- PTEN hamartoma tumor: PTEN
- mixed polyposis : GREM1
- serrated polyposis: RNF43,
- non-polyposis early CRC: POLE2, BRCA2, BRIP1, TP53비용 (2023년 현재): 1,014,403원의 50% (챠트에 검사 사유 기술 필요, 여러 상황에서 본인부담률이 달라짐)
*참고 APC mutation 706,511원 / STK11 mutation 308,347원GI 파트 교수님들께서 polyposis 환자가 발견되는 경우 유용하게 사용되실 수 있을 것으로 생각되며, 유전적 성향이 강력히 의심되는 대장암이 발견되는 경우 유용하게 사용될 수 있을 것으로 생각됩니다.
[2021-12-9. 애독자 질문]
교수님. 안녕하십니까. 지방 건진 센터에서 근무하는 XXX이라고 합니다. 위용종에 대한 궁금증이 있어 문의 드려 봅니다.
위에서 관찰되는 용종은 꼭 조직 검사를 해야 하는 것인지요? 저는 암이 의심되거나 암이 아니어도(암을 배제하기 위해서) 용종 절제술을 의뢰하기 위한 목적으로 위 용종에 대한 조직 검사를 합니다. HP나 fundic gland polyp처럼 너무 뻔하게 보이는 위 용종들은 근접 사진은 남겨두고 조직 검사는 하지 않은 채 나오곤 합니다.
그런데 추후에 검진 결과를 듣기 위해 재내원 하였을 때 (결과는 내과 외래에서 듣습니다) 용종에 대한 조직 검사를 하지 않았다고 화를 내시는 분도 계시고 고소한다고 엄포를 놓고 가신 분도 계셨습니다. 대장에서도 S-colon 이하에서 보이는 작은 HP는 굳이 제거하지 않는다고 알고 있고 위 용종은 대장 용종과 임상적 의미가 많이 다르다고 설명하는데 제가 잘못 알고 있는 것일까요? 그렇다고 해서 보이는 미란이나 발적, 용종 모두를 조직 검사해야 하는 것인지 최근 많이 혼란스러워 도움을 청해 봅니다.
[2021-12-10. 이준행 답변]
좋은 질문 감사합니다. 우리나라에서 위내시경 조직검사의 적응증은 정립되어 있지 않습니다. 그 결과 조직검사를 너무 많이 하시는 분도 계시고 너무 적게 하시는 분도 계십니다. 누가 옳고 그르고의 문제는 아니고 표준화가 되어 있지 않다는 의미입니다. 교육 훈련이 부족하다는 말과 같습니다. 일본에서는 건진 내시경에서 조직검사를 너무 많이 하지 않도록 지방정부 차원에서 모니터링을 하기도 합니다. 조직검사를 많이 하지 않고도 건진의 목적을 달성하기... 뭐 그 정도라고 이해하시면 됩니다. 육안 소견으로 guess하는 훈련을 많이 하면, 아주 많이 하면 조직검사를 줄일 수 있다는 의미이기도 합니다.
위에서 관찰되는 용종을 꼭 조직 검사를 해야 하는 것은 아닙니다. 선생님 말처럼 "암이 의심되거나 암이 아니어도(암을 배제하기 위해서) 용종 절제술을 의뢰하기 위한 목적으로 위 용종에 대한 조직 검사"를 하면 됩니다. 작은 hyperplastic polyp이나 fundic gland polyp처럼 너무 뻔하게 보이는 위 용종들은 근접 사진은 남겨두고 조직 검사는 하지 말자는 것은 좋은 정책입니다. 다만 처음 발견되었을 때에는 조직검사를 하는 것도 고려하시기 바랍니다.
"용종에 대한 조직 검사를 하지 않았다고 화를 내시는 분"도 나름의 입장이 있겠으나 다른 의료진의 견해를 존중하는 태도가 더 좋을 것 같습니다. "고소한다는 엄포"는 무시하면 됩니다. 의학적 판단의 이슈이지 법률적 다툼의 대상은 아닙니다.
우리나라에서 내시경을 가르치고 배우는 방식은 무척 후진적입니다. 체계적인 교육, 훈련, 토론, 연구가 없고 다들 제멋대로 검사하고 남을 탓하는 수준입니다. 하나씩 하나씩 발전시켜야 하겠습니다. 교육,훈련을 통한 질향상 노력이 절실합니다.
[2025-6-24] 목이 굵은 용종 절제술에 detachable snare를 잡아준 후 그 위를 절제하는 방법을 사용할 수 있습니다.
1) The pathology of gastric and duodenal polyps: current concepts Histopathology 2021;78:106
3) 용종절제술 도구. 성결 교수님
4) 용종증 폴립증후군 polyposis syndrome - 내시경세미나 강의록. 임종필. PDF 0.7M
5) Hamartomatous polyposis syndrome (PDF)
6) MUTYH 관련 폴립증 MUTYH associated polyposis (2023년 8월 내시경학회 교육자료)
7) Gastric polyps and dysplasia Paul J Kelly and Gregory Y Lauwers. PDF
 © 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.