 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [Gastric MALToma. MALT lymphoma. 말트 림프종. 말토마] - 終
[Gastric MALToma. MALT lymphoma. 말트 림프종. 말토마] - 終
1. 개념과 분류 Definition and classification
을지대학교 성결 - MALToma symposium (2022)
3. 병리 소견 Pathological findings
4. 병기 Staging - 私見
제15회 SMC 내시경세미나 - Single topic symposium on gastric MALToma
7. Helicobacter 음성 MALT 림프종 Helicobacter-negative MALToma
8. 골수 침윤 Bone marrow involvement
9. 환자 설명서 Information for patients
10. 애매한 경우 r/o early stage MALToma 혹은 suggestive (suspicious) of MALToma
11. 위 MALT 림프종 확진 (애매한 경우도 마찬가지입니다) 후 환자를 의뢰할 때에는 제균치료를 하지 말아주시기 바랍니다.
12. Collision 또는 MALToma and adenocarcinoma
13. FAQ
14. References
원발성 위장관 림프종은 주로 아래와 같이 정의됩니다.
Dawsons criteria for primary GI lymphoma (1) Originally used to define a primary intestinal lymphoma now modified to define gastric lymphomas also.
(2) Inclusion criteria: The organ is predominantly involved, and the intra-abdominal lymphadenopathy, if present, corresponds to the expected lymphatic drainage of the organ.
(3) Exclusion criteria: palpable subcutaneous nodule, mediastinal lymphadenopath, abnormal leucocytes on PBS/BM aspirate, splenic/hepatic involvement
원발성 위장관 림프종 중 위 MALT 림프종은 1983년 Isaacson과 Wright에 의해 체계화되었고, 최근 2008년 WHO 분류에서는 extranodal marginal zone B-cell lymphoma of MALT라는 이름으로 불리고 있습니다. 위 MALT 림프종의 진단과 치료에 대한 적지 않은 혼선이 있는데 이는 위 MALT 림프종에 대한 개념이 변하였기 때문입니다. 엄밀하지는 않지만 개념적으로 설명하면 다음과 같습니다.
위 MALT 림프종이라는 질환이 처음 정립될 무렵에는 B-세포 림프종을 (1) 고도 요소가 없는 MALT 림프종 (MALToma without high grade component), (2) 고도 요소를 가진 MALT 림프종 (MALToma with high grade component), (3) 미만성 거대 B-세포 림프종 (= 광범위큰B세포림프종, diffuse large B-cell lymphoma, DLBCL)의 3 군으로 구분하였습니다.
이 중 두 번째에 해당하는 고도 요소를 가진 MALT 림프종은 Helicobacter pylori 제균치료에 반응하는 경우도 있지만 (Regression of gastric high grade MALT lymphoma after H. pylori eradication. Montalban C. Gut 2001), 대부분은 DLBCL와 비슷한 경과를 보입니다. 따라서 최근에는 고도 요소가 없는 MALT 림프종만을 extranodal marginal zone B-cell lymphoma of MALT라고 부르고 나머지 두 군은 DLBCL로 통칭하고 있습니다. 2013년 ESMO 가이드라인(Zucca. Ann Oncol 2013)에는 다음과 같은 언급이 있습니다. "It should be noted that the term 'high grade MALT lymphomas' is no longer accepted in the current WHO classification, hence cases with solid or sheet-like proliferation of transformed large cells have to be diagnosed as diffuse large B-cell lymphoma."
병리학교과서에서는 위장관 DLBCL를 MALT 림프종 요소를 가진 경우와 MALT 림프종 요소가 없는 경우로 나누기도 합니다.
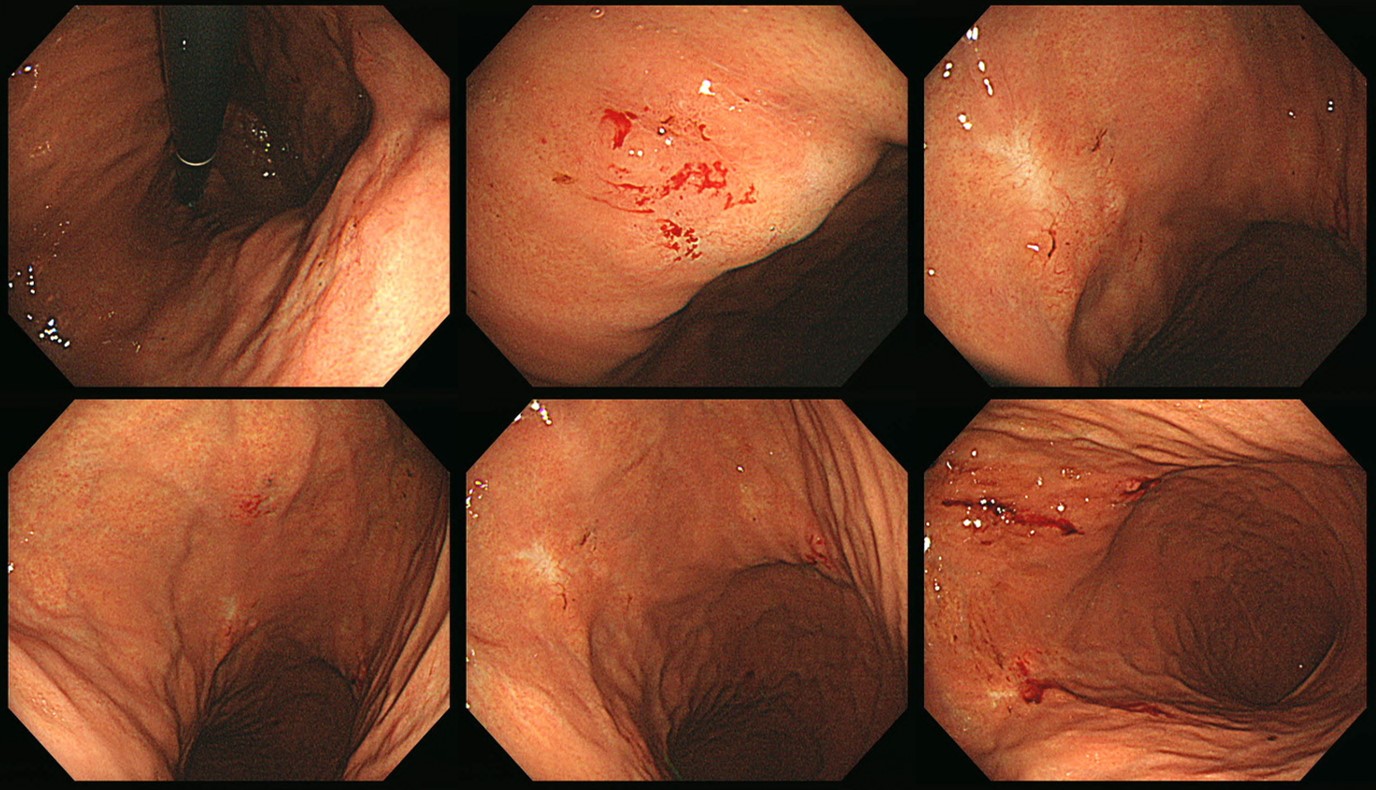
EndoTODAY MALToma의 내시경 소견으로 옮겼습니다.
 3. 병리 소견. Pathology of gastric MALToma
3. 병리 소견. Pathology of gastric MALToma
위 MALT 림프종의 병리학적 특징은 다음과 같은 5 가지 소견으로 정리할 수 있습니다.
Mantle cell lymphoma를 배제하기 위하여 cyclin D1 염색 음성임을 강조하는 전문가도 있습니다. 병리의사들도 경험이 쌓이면서 최근에는 cyclin D1 염색은 자주 시행되지 않는 것 같습니다.
2016년 한 리뷰에서는 아래와 같이 요약하였습니다 (Hu. Biomark Res 2016).
2022년 5월 내시경세미나 병리강의를 듣고 아래와 같이 요약해 보았습니다.
[Cases]
다른 환자. 뚜렷한 lymphoepithelial lesion by MALToma
다른 환자. 뚜렷한 lymphoepithelial lesion by MALToma
다른 환자. 뚜렷한 lymphoepithelial lesion by MALToma (cytokeratin AE1.AE3 immunohistochemistry)
[Advances in surgical pathology. Gastic cancer (2011)]
Expansion of the marginal zone of the hyperplatic lymphoid follicle, dense lymphoid infiltrate composed prodominantly small B cells, increase in plasmacyoid lymphocytes, dropping out of gastric glands, and conspicuous lymphoepithelial lesions (LELs) are all morphological features that favor MALT lymphoma.
Microscopically, MALT lymphoma is morphologically heterogenous. The characteristic lymphoma cells are small to medium in size and have a bland appearance with relatively increased cytoplasm, slightly irregular nuclei, moderately dispersed chromatin, and incounspicuous nucleoli, resembling centrocytes. The relative abundant, pale cytoplasm allows the cells to exhibit a "monocytoid" morphology. (ample clear space between the nuclei of the adjacent lymphoma cells) The neoplastic cells can also infiltrate the gastric glands and forms clusters within the glandular epithelium, fostering "lymphoepithelial lesions". The characteristic LELs can be highlighted by staining for pancytokeratin.
The cells are almost always positive for CD19, CD20, CD22, and CD79a and show surface immunoglobulin light chain kappa or lambda restriction. They are frequently positive for CD43. Typically negative for CD5 and CD10, an immunophenotype differs from those of most other small B-cell lymphomas (chronic lymphocytic leukemia/small lymphocytic lymphoma, follicular lymphoma, and mantle cell lymphoma). The neoplasic B cells often are accompanied by plasmacytic differentiation as well as monoclonal plasma cells. Although primary lymphoplasmocytic lymphoma in the stomach is much rarer than MALT lymphomas, it has been reported (Okuda 2001). Because of the overlapping features, differentiating between these two diseases is extremely difficult. In addition to Waldenstrom macroglobulinemia, which is often associated with lymphoplasmocytic lymphoma, cytogenetic analysis is helpful in differentiating these two lymphomas.
YouTube link Minimal panel for MALToma로 CD3, CD20, CD43, cyclin D1를 추천
[한 병리학자의 working format (하상윤 2020)]
| Pathology | Suggestion |
| Dense lymphocytic infiltration with definite LEL | MALToma |
| Dense lymphocytic infiltration with equivocal LEL | s/o MALToma F/U biopsy or cytoketatin staining |
| Lymphocytic infilation without LEL | Gastritis with lymphoid aggregate |
| Cytological atypia or large cell component | CD3, CD5, cyclin D-1, Bcl-2, Ki-67 |
[Lymphoid hyperplasia, lymphoid aggregate]
조직검사에서 lymphoid hyperplasia나 lymphoid aggregate로 나오는 경우가 많습니다. 이런 경우 내시경 육안 소견이 가장 중요할 것 같습니다. DLBL이 의심되면 반드시 재검이 필요합니다. MALToma가 의심되면 short-term follow up이 필요합니다. 내시경 소견이 단순 위염인데 우연히 lymphoid hyperplasia나 lymphoid aggregate로 나오는 경우는 임상적 의의는 크지 않습니다. 12개월 (혹은 6개월) 후 재검 정도면 충분하지 않을까요? 물론 헬리코박터가 양성이면 치료를 하고 있습니다.
M/43 (2019). 의뢰 후 조직검사에서 "Chronic gastritis, inactive with lymphoid aggregate. No H. pylori identified." 소견이었고 1년 후 내시경 재검을 권하였습니다.
[Cyclin D1 immunohistochemistry가 매우 유용하였던 mantle cell lymphoma 증례]
The histological diagnosis of gastric MALToma and gastric mantle cell lymphoma may be confusing. The most distinguishing feature is cyclin-D1 positive in mantel cell lymphoma and cyclin-D1 negastive in MALT lymphoma. However, immonohistochemical staining of cylin-D1 is not routinely done for typical MALToma cases.
In about 15 years ago, we experience a case with mantle cell lymphoma, which was considered as MALToma of the stomach. Based on the gastric forcep biopsy result, H. pylori eradication therapy was done under the impression of gastric MALToma.
A few months later, the patient suddenly developed ileocecal intussusception and surgical resection was done.
To our surprise, the final pathology was cyclin-D1 positive mantle cell lymphoma.
When we reviewed the original gastric specimen, it was concluded that the initial correct diagnosis was gastric mantle cell lymphoma. Cyclin-D1 immunohistochemistry is still very useful for cases with uncertain pathologic diagnosis.
실제로 이와 같은 소견들은 디지털적인 단계보다는 아나로그적인 스펙트럼을 가지고 있으므로 Wotherspoon 등이 나눈 scoring system이 자주 사용되었습니다. 2010년 경부터는 잘 씌이지 않고 있습니다만.
Wotherspoon 3이나 4가 나오면 고민입니다. 한 리뷰에서는 PCR로 평가한 monoclonality로 암진단을 한다고 되어 있습니다. 그러나 이 또한 표준적인 방법은 아닙니다. 저는 병리과 선생님을 찾아가서 함께 슬라이드를 보면서 고민하는 방법을 택합니다. PCR보다 낫다고 생각합니다.
MALToma의 특징적인 병리소견 중 하나가 plasma cell infiltration입니다. 과거 plasmacytoma로 분류된 위암 중 상당부분이 현재의 개념으로는 plasma cell predominant type의 MALToma입니다. 첫 병원에서 plasmacytoma로 판단하여 수술이 권유되었으나 두번째 병원에서 plasma cell predominant type의 MALToma로 진단되어 제균치료 후 완전관해상태로 8년 이상 관해상태인 증례를 소개합니다.
관련자료를 하나 소개합니다 (Kodama. Am J Med 1999)
"Approximately one third of all cases of gastric MALToma show variable degrees of plasma cell differentiation, occasionally plasma cells constitute the major population in the tumor. As surgical resection has been the standard treatment for gastric plasmacyotoma, this case highlights the need for caution. If H. pylori infection is found in a patient with a gastric plasmacytoma, it should be eradicated as a first line of therapy before surgery is considered."
[Signet ring-like cells in MALToma]
MALToma에서 signet ring-like cell이 관찰될 수 있습니다.
Carcinoma-like signet-ring cells in MALT lymphoma (Am J Surg Pathol 1996)
Abstract: We noticed the presence of epithelial signet-ring cells (SRCs) in a proportion of primary gastric B-cell lymphomas, and in some endoscopic biopsies we found it difficult to decide whether they represented an associated carcinoma. To evaluate the frequency and nature of this phenomenon, we reviewed 108 stomachs resected for primary lymphoma, including 70 mucosa-associated lymphoid tissue (MALT) and 38 non-MALT lymphomas. We found SRCs, either isolated or grouped in clusters, in 26 of 70 MALT lymphomas. The SRCs were always localized in the superficial portion of the lamina propria and associated exclusively with lymphomatous areas. Isolated and scarce SRCs were also found in four of 22 cases of polyclonal atypical lymphoid hyperplasia. Our data suggests that SRCs occurring in gastric MALT lymphomas represent a particular type of LEL in which the foveolar cells disaggregated by the lymphomatous infiltration acquire a globoid, signet-ring appearance. These "foveolar" LELs are found in 37% of MALT lymphomas and are usually associated with the more classic and constant "neck" LELs, which are localized between the foveolae and mucopeptic glands. An awareness of the existence of the foveolar LEL may help avoid overdiagnosis of SRC carcinoma on gastric endoscopic biopsies.
[Immunoglobulin analysis]
The neoplastic cells of which MALT lymphomas are composed express B-cell antigens and show monotypic immunoglobulin expression with light-chain restriction.
The most definitive and useful immunophenotypic determination in diagnosing lymphoma is light chain restriction. Immunoglobulin light chain restriction is, with rare exceptions, considered diagnostic for B-cell neoplasia... In reactive lymphoid populations there is a mixture of kappa and of lambda positive cells, with cells expressing kappa light chains outnumbering cells expressing lambda light chains. Kappa expression is also more common than lambda in lymphoid neoplasms with the exception of hairy cell leukemia and mantle cell lymphoma. Light chains are not expressed on the surface in plasmacytoid lesions and in early B-cell lesions. With higher grade B-cell lymphomas there is a decreased incidence of light chain expression. Monoclonal B-cells express a uniform quantity of surface Ig while polyclonal B-cells have a heterogeneous surface Ig expression. This results in a narrower distribution of staining intensity with anti light chain reagents in monoclonal B-cells in comparison to polyclonal B-cells. (Sentence source)
면역 글로불린의 경쇄(light chain, kappa 혹은 lamda) 양성 세포의 비율에 편중이 보이며 kappa/lamda=0.2 이하 또는 10 이상이라며 종양성이 강하게 의심됨다. 강한 편중이 확인되는 현상을 경쇄 제한 (light chain restriction)이라고 한다. 형질세포로의 분화를 보이는 세포가 적은 경우에는 뚜렷하지 않다.
* 참고: Molecular pathogenesis of MALT lymphoma Gastroenterol Res Pract. 2015
위 MALT 림프종은 무증상 성인의 건강검진에서 발견되는 경우가 많고, H. pylori 제균치료로 호전되는 예가 80% 이상이므로 staging을 소홀히 하기 쉽습니다. 그러나 늘 조심해야 합니다. 내시경, 조직검사, CT는 기본입니다.
문제는 'EUS와 골수 검사가 필요한가?'입니다. 표준적인 문헌에서는 당연히 두 검사를 모두 하는 것으로 되어 있습니다. 그러나 제가 근무하는 병원에서도 교수들 사이에 의견 통일이 되어 있지 않습니다. 안하시는 분이 더 많지만 하시는 분도 계십니다.
건진에서 발견되는 경미한 위 MALT 림프종 환자에서 모두 EUS와 bone marrow가 필요하다고 생각되지는 않습니다. 정확한 기준은 없습니다만, 저는 대략 20%는 EUS나 골수검사를 하고 있고 나머지는 검사하지 않고 있습니다. 정확한 기준은 없이 치료하고 있는데 아직까지 별 문제는 없었습니다. 언젠가 명확히 정리해야 할 이슈라고 생각하지만 아직 참고할 문헌도 없습니다. 완전히 임상가의 감(感)에 의존해서 선택한다고 보면 크게 틀리지 않습니다. 의사 스타일 말입니다 (물론 저는 담백 스타일입니다).
MALToma 중 stage가 높은 사람이 드물기 때문에 staging workup을 게을리 하는 경우가 있습니다. 그러나 간혹 다발성 복강내 전이가 발견되기도 합니다. H. pylori 제균치료는 해야 하겠지만 이것으로는 부족한 경우입니다. 대부분 systemic chemotherapy가 필요합니다.
Fundus gastric MALToma였습니다. 병리는 두번 모두 low grade MALToma로 나왔고 Hp (+)였습니다. 아쉽게도 복강내 다발성 림프절 전이가 있었습니다. 그런데... 환자가 16개월 전 내시경 검사를 받은 적이 있다고 하여 과거 사진을 확인한 바 위 fundus의 fold가 두꺼워진 부위가 있었습니다. 위 fundus fold가 두꺼워진 경우는 항상 조심스럽습니다. Varix 일 수 있기 때문입니다. 그래서 조심조심 잘 살펴보는 수밖에... (2016, M/56)
[私見]
임상연구 논문을 작성할 계획이면 EUS를 하는 것이 좋습니다. EUS 없이는 논문쓰기 어렵습니다. 그러나 환자 치료에 집중할 계획이면 대부분의 경우 EUS는 필요하지 않습니다. Depth of invasion과 무관하게 대부분 제균치료를 할 것이기 때문입니다. EUS 결과는 치료 반응 예측에 다소 유용하다는 논문도 있지만, 육안소견만으로도 상당히 정확히 예측할 수 있는 것 같습니다. 육안소견에 EUS 소견을 더할 때 더 도움되는지는 아직 명확하지 않습니다. 저는 비급여 검사를 무척 싫어하기 때문에 여간해서는 EUS를 시행하지 않고 있습니다. 득에 비하여 너무 비싼 것 같아서...
아래는 한 건진센터에서 외래로 MALToma 환자를 의뢰한 후 추적한 결과입니다. 4명의 의사에게 의뢰되었는데 모두 스타일이 달랐습니다. 3분은 아주 간략히 검사하는 스타일이고 1분은 일반적인 lymphoma와 동일하게 아주 많은 검사를 하셨습니다. Hp 음성 MALToma의 초치료로 RT를 선택하신 분도 계십니다. 이게 현실입니다. 다 다릅니다. 저야 아주 간략하게 검사하는 스타일입니다.
미국에서는 gastric MALToma에 대하여 제가 상상할 수 없을 정도의 많은 검사를 guideline에서 언급하고 있습니다. 아래는 2025년 NCCN 가이드라인입니다. 과잉도 이런 과잉이 없다 싶습니다. 물론 우리나라에서 이 많은 검사를 다 하면 엄청 삭감될 것입니다. 사실 필요하지도 않고요...
제15회 SMC 내시경세미나 - Single topic symposium on gastric MALToma
병기결정을 위한 검사 (CT, EUS, 골수검사 등) 후 점막이나 위점막하층에 국한된 MALT 림프종으로 진단되고 H. pylori 감염이 동반되어 있으면 H. pylori 제균치료를 시행합니다.제균치료로 인하여 완전관해에 도달하는 비율은 대략 80% 정도로 알려져 왔습니다. 최근에는 건강검진을 통하여 경미한 MALT 림프종이 많아져서 과거보다 제균치료의 효과가 더욱 좋다는 견해가 있습니다.
2005년 이전의 초창기 protocol. Proper muscle 이상을 침윤한 경우에는 항암치료를 선택하는 방식
최근 사용하고 있는 protocol. Stage IE2 (proper muscle 이상의 침윤)에서도 대부분 일단 H. pylori 제균치료부터 시행하는 방식
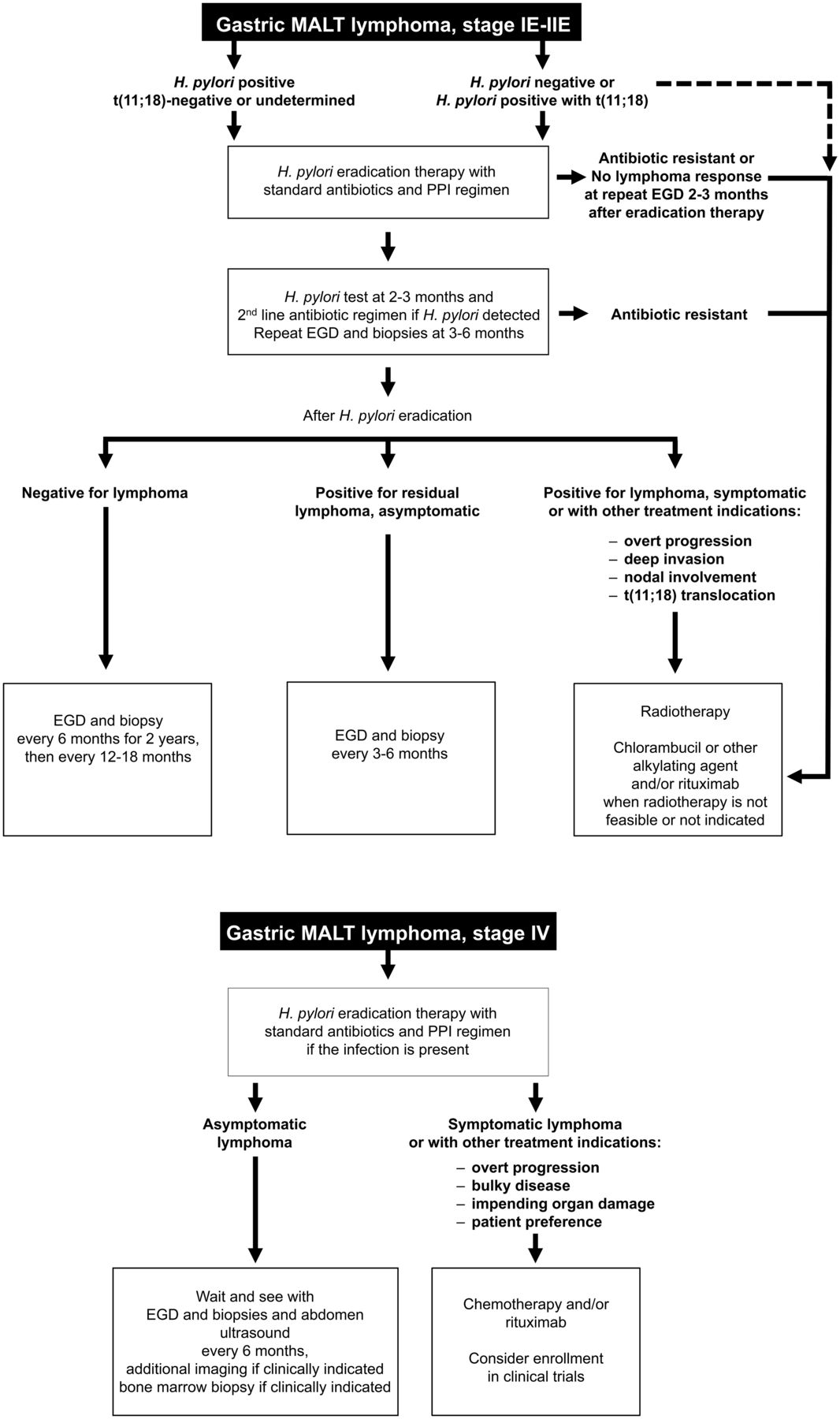
ESMO 2013년 가이드라인 (Zucca. Ann Oncol 2013 - free PDF). Stage IE에서는 depth of invasion을 고려하지 않고 H. pylori 제균치료를 하도록 권하고 있습니다. 심지어는 intra-abdominal node가 있는 stage IIE에서도 H. pylori 제균치료를 권하고 있습니다.
1차 제균치료 failure로 2차 제균치료를 시행하였고 이후 호전되었던 gastric MALToma
Giemsa staining과 UBT는 음성이었으나 serology는 양성이었으므로 제균치료하였고 이후 호전된 gastric MALToma
제균치료 후 관해 여부는 내시경과 조직검사 소견을 종합하여 판단합니다. 물론 조직검사가 더 중요합니다. 그런데 2000년 경부터 GELA staging system이라는 것이 소개되어 큰 혼란을 만들고 있습니다. 너무 많은 문제가 있는 시스템이지만 특히 다음 두 가지는 정말 골치입니다. (1) pMRD (probable minimal residual disease)가 관해(remission)로 해석된다는 것입니다. pMRD를 그대로 번역하면 "아마도 암이 조금 남아있는 것 같다"인데 이를 관해로 해석해야 하다니...... 이를 이해할 수 있는 환자나 의사는 없습니다. 명칭을 바꿔야 한다고 생각합니다. (2) NC (no change)입니다. 언끗 생각이 "변화가 없으니 좋은 것이구나"입니다. 그러나 전혀 호전이 없다는 것입니다. 즉 매우 나쁜 것이 no change입니다. 저도 헷갈린 경우가 있었습니다. 명칭을 바꿔야 한다고 생각합니다. 여하튼 어떤 병리과 의사가 한심한 system을 제안하였는데 너무 많이들 사용하고 있는 것 같습니다.
GELA에 따른 결과에서 pMRD라는 용어때문에 '눈으로 보기에는 좋아졌는데 암이 남아있을 수 있다'는 설명을 듣고 도저히 이해할 수 없어서 이차 의견을 듣기 위하여 먼 병원을 찾아왔던 환자 (2013년 증례).
MALToma가 일단 관해에 도달하였다가 재발하였을 때 선택할 수 있는 방법 중 하나는 wait and see입니다. 그러나 첫 치료 단계에서 한번도 관해에 도달하지 않았던 환자에서 내시경 소견이 좋아졌다는 이유만으로 조직에서 MALToma가 나오는데 계속 기다려도 좋을지 의문이 아닐 수 없습니다. 문헌이나 저의 임상 경험 상 급할 것은 없다고 생각합니다만 환자의 불안을 잠재울 방법이 없습니다. 저는 충분히 기다렸는데도 조직학적으로 호전(pMRD 혹은 CR)되지 않으면 대부분 방사선 치료를 권하고 있습니다. 방사선 치료의 효과가 좋고 toxicity는 심하지 않기 때문입니다. 환자 입장에서는 치료방법이 있는데도 단지 내시경 소견이 좋아졌다는 이유만으로 암(癌)을 가지고 산다는 심리적 부담이 더 크지 않을까요? (2020-10-10. 이준행)
pMRD가 임상적으로는 관해로 해석되는 모순을 환자에게 설명하기가 쉽지 않습니다. 저는 이와 같이 GELA 판정 기준표를 보여주고 4단계 중 2단계가 나왔다고 설명하고 있습니다. (2017-8-1)
제균치료 후 관해에 도달하는 시간은 환자에 따라 차이가 큽니다. 몇 년 전 아산병원 자료(Hong SS. Helicobacter 2006)에 의하면 관해까지의 중앙값(median)은 3개월이었습니다. 그러나 1년 이상 기다린 후에야 관해에 도달하는 경우도 상당수 존재합니다.
50대 여성. MALT 림프종 제균치료 후 3년 만에 histological complete remission에 도달
제균치료로 관해에 도달하지 않는 예는 대부분 (1) 점막하층을 넘어 침범되어 있거나, (2) 고도 요소를 가지고 있거나, (3) 내시경초음파에서 위 주위 림프절이 침범되어 있거나, (4) t(11;18)(q21;q21)와 같은 염색체 이상이 존재하는 경우입니다. 아래는 삼성서울병원에서 MALT 림프종 환자의 임상경과를 요약한 내용입니다.
조직검사와 initial staging workup이 완벽하지 않기 때문에, 그리고 약간 깊어보여도 처음부터 항암치료를 하는 것은 아쉽기 때문에 애매한 경우에는 H. pylori 제균치료부터 해 보는 경우가 있습니다. 좋아지는 예도 있고 그렇지 못한 예도 있습니다. 약간 깊어보이는 증례에서는 일단 H. pylori 제균치료를 시행한 후 단기 추적관찰에서 병소의 악화여부를 보는 것도 유용한 전략입니다.
Hp 제균치료 3개월 후 내시경에서 매우 악화되어 의뢰된 환자입니다. 항암치료를 하였습니다.
다소 애매하여 Hp 제균치료 3개월 후 추적관찰을 하였으나 병소가 악화되었기 때문에 항암치료를 시행하였습니다.
처음부터 제균치료에 반응하지 않는 MALT 림프종에 대해서는 방사선치료(30 Gy 정도)가 가장 많이 이용되며 드물게 항암화학요법이 사용되기도 합니다. (참고문헌 1, 참고문헌 2)
RT 후 호전된 증례입니다.
Hp 양성 MALToma였습니다. 제균치료를 하였고 충분히 기다렸는데 호전되지 않았습니다. RT를 하였고 완전 관해에 도달하였고 5년 이상 재발 없이 잘 지내고 계십니다.
그러나 모든 환자에서 방사선치료과 효과적인 것은 아닙니다. 항암치료가 필요한 경우도 있습니다.
헬리코박터 제균치료 후 관해에 도달하지 않았는데 추가 치료를 받지 않겠다고 하셔서 경과관찰을 하였던 환자도 있었습니다.
제균치료 후 보통 1-1.5년을 기다립니다. 그러나 중간에 악화소견이 있어 방사선 치료로 변경하는 예도 있습니다. 기다린다는 것은 환자나 의사나 모두 어려운 결정입니다.
ECR 013 Gastric MALToma treated by RT
MALToma에 대한 H. pylori 제균치료 후 추적내시경에서 원래 MALToma로 진단되었던 부위 이외의 다른 곳에서 multifocal atrophic area들이 관찰되는 경우가 있습니다 (흰 동그라미).
이는 첫 내시경 당시 발견되지 못하였던 다발성 MALToma 병소들이었던 것으로 추정됩니다. 비록 내시경에서 한 병소만 발견되었더라도 자세히 살펴보면 다른 곳에서 작은 MALToma 병소가 scattered 되어 있는 예가 많다는 것입니다. 이 때문에 첫 진단 시 수십개의 random biopsy를 하자고 주장하는 과거 교과서도 있었습니다. 저는 가장 현저한 병소를 target으로 치료하면 사소한 병소는 함께 좋아지는 것을 경험하고 있습니다. 따라서 첫 진단 시 수십개의 random biopsy를 위한 내시경 재검은 하지 않고 있습니다. 필요없는 과잉 검사라고 생각하고 있습니다.
요컨데 MALToma 환자의 추적 내시경에서 multifocal atrophic area가 발견된다고 놀라지 마시라는 이야기입니다. 원래 patchy distribution 하는 병이니까요.
[GELA 분류의 한심함에 대하여]
제가 강조하고 싶은 것은 GELA system의 용어에 대한 것입니다. 의학에서 "No change"는 항상 좋은 뜻으로 씌여 왔습니다. Cyst의 크기가 변하지 않았다, Lung nodule의 크기 변화가 없다... 등 no change는 문제가 없다는 뜻으로 씌여 왔습니다. 그런데 GELA system에서 no change는 하나도 변하지 않았다. 즉 매우 나쁘다는 뜻입니다. 이로 인한 실수도 적지 않습니다.
pMRD (probable minimal residual disease)도 마찬가지 문제가 있습니다. 임상적으로 remission으로 판정하는데 조직학적 진단명은 "아마도 약간 남아있는 것 같다 (pMRD)"이니 앞뒤가 안 맞는 것입니다. 따라서... GELA system에서 사용되고 있는 모호한 용어를 대신할 새로운 용어가 필요합니다. 병리의사들의 분발을 촉구합니다.
제균치료로 관해에 도달한 환자의 재발률은 10% 정도입니다. 재발 환자의 상당수는 H. pylori 양성입니다. 제균치료를 다시 시도하는 것은 유용한 전략입니다.
일단 관해에 도달한 환자의 추적관찰 중 작은 병소가 발견되고 조직학적으로 재발로 판단된 경우라도 치료를 서두를 필요는 없습니다. EMSO 2013년 가이드라인 (Zucca. Ann Oncol 2013)에는 다음과 같이 언급되어 있습니다. "In the case of persistent but stable residual disease or histological relapse (without distant dissemination and/or gross endoscopic tumour), a watch-and-wait policy appears to be safe".
그러나 현실 의료에서는 국소 재발인 환자를 대상으로 가이드라인에 언급된 watch-and-wait를 설명하고 아무 것도 하지 않고 추적관찰하는 것은 쉬운 일이 아닙니다. 특히 암이면 벌벌 떠는 우리나라 국민 정서상 watach-and-wait를 하기는 매우 어렵습니다. 그래서 재발 예는 대부분 방사선 치료가 이루어지는 것이 현실입니다. 저도 몇 분을 제외하고는 방사선 치료를 했습니다. 몇 분은 치료하지 않았는데 큰 문제 없이 잘 지내시고 계십니다.
2017년 2월 대한소화기내시경학회 증례에서도 MALToma 재발예에 대한 방사선 치료가 소개되었습니다.
2017년 7월 대한상부위장관,헬리코박터학회 4차 교육자료에서는 MALToma 재발에 대한 watch-and-wait 전략을 적용한 증례가 소개되었습니다.
저는 외래에서 환자에서 아래와 같이 설명하고 있습니다 (2016년 2월 현재).
재발 위 MALT 림프종의 치료 전략은 세 가지입니다.
1. careful wait and see
- 지금처럼 지켜보는 것입니다. 질병 자체가 매우 천천히 변화하는 특징이 있으므로 수년 이상 이 상태로 지속되는 분이 많습니다. 2013년 유럽 가이드라인(Zucca. Ann Oncol 2013 )에도 watch and wait가 언급되어 있습니다.
2. 방사선 치료
3. 항암 치료
- 방사선 치료나 항암 치료와 같은 적극적인 치료르 고려할 수 있습니다. 과거에는 이러한 전략을 많이 사용하였습니다. 그런데... 림프종이 빨리 자라는 타입에서는 방사선 치료나 항암치료의 효과가 좋은 반면 천천히 자라는 타입은 오히려 효과가 떨어지는 경향이 있습니다. 즉 치료를 해도 계속 림프종이 나오는 환자가 적지 않다는 것입니다.
저희는 최대한 자세히 설명드리고 환자의 의견을 존중한다는 입장입니다. 생각할 시간을 갖고 1주일 후 외래 방문해 주시기 바랍니다. 2차 의견을 원하시면 방사선 종양학과로 의뢰하여 의견을 듣도록 해 드릴 수 있습니다.
For advanced diseases, rituximab (a monoclonal CD20 antibody) alone or in combination with other chemotherapeutic agents may be warranted.
[위 MALT 림프종 치료 후 extragastric DLBCL]
위 MALT 림프종에 대한 헬리코박터 제균치료 후 위 MALT 림프종은 호전되었으나 수 년 후 extragastric DLBCL가 발견되는 예가 있습니다. 따라서 위내시경 추적검사와 함께 CT 검사가 꼭 필요하다고 생각합니다.
참고: 20205년 KSGE 증례: 방사선 치료 후 재발된 위 MALT 림프종 Recurrence after radiotherapy for gastric MALT lymphoma
Helicobacter 음성 MALT 림프종은 흔하지 않지만 고민되는 상황입니다. 10여년 전 삼성서울병원 fellow 이선영 선생님(현 건국대 교수)의 리뷰를 소개합니다. 이후 2015년 경 일본에서 새로운 개념이 정립되고 있습니다. 아래 이선영 교수님의 강의를 참고하세요.
Helicobacter 음성 MALT 림프종으로 의뢰된 환자라고 하더라도 몇 가지 검사를 해 보면 Helicobacter 양성으로 나오는 경우가 많습니다. 따라서 한 검사에서 음성이라는 이유로 쉽게 'Helicobacter 음성 MALT 림프종'으로 이름 붙이지 않기를 바랍니다. 최근에는 꼭 H. pylori serology를 하고 있습니다. Serology까지 음성이어야만 진정한 H. pylori 음성 MALToma 아닌가 생각합니다. (2017-1-24)
전형적인 MALT 림프종입니다. 그런데 외부 조직검사와 의뢰 후 재검 Giemsa staining에서 Hp 음성으로 나왔습니다.
Serology와 UBT를 처방하였습니다. 둘 다 양성으로 나왔습니다.
Giemsa (-), UBT (-), serology (+). 이 환자는 H. pylori 음성 MALToma로 분류하면 안 될 것 같습니다.
MALToma에서 하나라도 Hp (+)이면 Hp-related MALToma로 진단하고 있습니다. Giemsa staining 음성, UBT 음성, CLOtest 음성이었지만 H. pylori serology는 양성이었습니다. Pepsinogen 1 = 33.3, pepsinogen 2 = 14.9, pepsinogen 1/2 ratio = 3.1 이었습니다. 제균치료를 하였고 깨끗이 좋아졌습니다. 하나라도 양성이면 양성입니다.
수 년 전 Hp 음성 MALToma로 진단을 듣고 RT 후 후전된 환자가 수 년 후 검진에서 MALToma 재발은 없는데 조직검사에서 Hp gastritis가 나와 의뢰된 환자가 있었습니다. 처음 진단 시 Hp에 대해서는 조직검사와 호기검사가 시행된 상태였고 두 가지 검사가 음성이라는 것을 근거로 Hp 음성 MALToma로 진단된 상황이었습니다. 처음 진단시 Giemsa staining, CLOtest, serology를 해 보았다면 어떠하였을까 생각해 보았습니다.
저는 Helicobacter 음성 MALT 림프종이라고 판단된 경우라도 일단 제균치료를 시행한 후 경과관찰을 합니다. Helicobacter 음성이므로 세 가지 이슈가 발생합니다. (1) 약제의 선택. 보통 한번의 제균치료를 적용하므로 triple therapy 보다는 quadruple therapy를 적용하는 경우가 많습니다. (2) 추적관찰. 처음부터 Helicobacter 음성이므로 UBT를 해도 알 수 없습니다. 그러나 다른 좋은 지표가 없으므로 UBT와 내시경 육안소견 관찰 및 조직검사를 통하여 상황을 재평가하고 있습니다. (3) 언제까지 관찰할 것인가? Helicobacter 양성 MALT 림프종에서는 12-18개월까지 관찰합니다. 그러나 Helicobacter 음성 MALToma를 이렇게 오래 관찰해도 좋은지 자료가 없습니다. 보통 maximum 1년까지 관찰하는 전문가가 많습니다. 이 정도 기다렸는데, 호전이 없으면 RT를 권합니다. 호전이 있을 확률이 30-50%이므로 대략 절반은 RT로 넘어가고 절반은 장기 추적관차를 한다고 이해하면 크게 틀리지 않습니다.
Hp 음성 MALT 림프종 환자로 RT 후 호전된 환자입니다.
그런데 추적내시경 검사의 결과가 MALToma로만 되어 있습니다. 결과만 보면 "재발인가?" 의심할 수 있습니다. MALT 림프종이었으나 치료 후 호전된 환자의 내시경을 할 때에는 'Remission after treatment for MALToma' 혹은 'MALToma in remission'으로 impression을 붙여주시기 바랍니다.
2016년 아산병원에서 H. pylori 음성 MALT 림프종 치료에 대한 대규모 임상연구를 발표하였습니다 (Gong EJ. Gut Liver 2016).
같은 병원에서 2023년 ESD로 치료한 H. pylori 음성 MALT 림프종 6예에 대한 case series를 발표하였습니다.
[2018년 7월 9일 헬리코박터 집담회 이선영 교수님 강의. Hp negative MALToma]
Hp negative MALToma의 일부에서 rapid progression 하는 형태가 있으니 주의가 필요합니다. API2-MALT1 chimera가 없으면서 SMT 처럼 보이는 형태가 나쁘다고 합니다.
MALToma의 staging workup에 골수검사가 들어있습니다. 아주 드물게 골수 침윤이 있는 것으로 나옵니다. 그러나 그 임상적 의의는 명확하지 않습니다. Gut and Liver 2014년 11월호에 삼성서울병원 민병훈교수께서 위 MALT 림프종의 골수침윤에 대하여 분석한 논문이 실렸습니다 (link). 결론은 아래와 같았습니다.
"It might be beneficial to perform BM aspiration and biopsy as a part of staging work-up only in patients with risk factors for advanced disease such as H. pylori negativity"
그렇습니다. 모든 위 MALToma 환자에서 골수검사가 필요한 것은 아닙니다. Helicobacter 음성이거나 다른 고위험 인자가 있는 경우에만 시행하여도 무방하다고 생각합니다. 연구 대상이었던 194명 중에서 골수침윤이 있었던 환자는 단 1명이었습니다.
이 논문에 대하여 가톨릭대학교 정대영 교수님 팀에서 editorial을 실었습니다. 그 결론도 비슷하였습니다.
This article gives us meaningful evidences. In Korea, it is once in a blue moon that gastric MALT lymphoma involves bone marrow. Patient with bone marrow involvement has abdominal lymph node metastasis, even without mediastinal lymph node metastasis. Helicobacter infection negativity is related with abdominal lymph node metastasis and possibly be with bone marrow involvement. We need properly adjust Korean guideline of gastic MALT lymphoma based on Korean database. Abscence of Helicobacter infection, t(11;18)(q21:q21), depth of invasion, abdominal lymph node metastais should be considered risk factors for bone marrow involvement. The cost and benefit of bone marrow aspiration and biopsy should be balanced, and the scale of ours seems to be tipped in favor of "doing in highly selected cases."
2013년 아산병원에서 좋은 보고가 나왔습니다 (Won. Helicobacter 2013). 골수 침윤도 그 정도에 따라 의미가 다르다는 것입니다. Subtle하면 크게 걱정하지 말라는 것입니다. 저희의 임상 경험과도 일치하는 내용인지라 타당한 결론이라 생각합니다. 결론 부분과 대표 그래프를 옮깁니다. 참고로 2016년 아산병원 소화기내과에서 발표한 위 MALT 림프종 694명 중 골수검사를 하였고 추적관찰이 가능한 440명을 분석한 논문에서도 비슷한 결론을 보였주었습니다 (Gong EJ. Scand J Gastroenterol 2016).
Patients with BM(+) MALT lymphoma showed significantly worse PFS than those with subtle CD20 positivity and BM(-) MALT lymphoma, but the PFS of patients with subtle CD20 positivity MALT lymphoma was not significantly different from that of those with BM(-) MALT lymphoma
. Increased numbers of BM T cells in MALT lymphoma patients might be suggestive of a worse prognosis.
Gong EJ. Scand J Gastroenterol 2016
골수침윤이 있더라도 대부분 제균치료를 초치료로 선택하였고 outcome은 favorable 했습니다. Gong EJ. Scand J Gastroenterol 2016
2016년 한 리뷰에서는 림프절 침범이 없으면 골수검사는 필요하지 않다고 적고 있습니다 (Hu. Biomark Res 2016).
As soon as a pathological diagnosis of gastric MALT lymphoma is established, clinical staging of the disease should be performed. The modified Ann Arbor (Musshoff) system is recommended for the staging. The majority of cases with gastric MALT lymphoma are in the early stage of disease, with lymphoma limited to the gastric mucosa, submucosa (stage I1E) and less commonly, in the superficial layer of the muscularis propria (stage I2E). Endoscopic ultrasound for the detection of lymphoma invasion of the stomach wall has been used in European countries. Routine abdominal CT scan is recommended for possible regional gastric lymph node involvement (stage II1E). Bone marrow involvement is uncommon, and routine bone marrow biopsy for staging is not recommended for patients with negative regional lymphadenopathy.
2018년 국립암센터의 보고(Gut Liver 2018)에 의하면 골수 검사를 시행하였던 92명 중 4명(4.3%)에서 골수 침윤이 있었습니다. 그러나 모든 환자가 적절한 치료 (제균치료 혹은 방사선치료 혹은 항암치료) 후 모두 임상적 관해에 도달했습니다.
METHODS: In total, 132 patients who were diagnosed with gastric MALT lymphoma at the National Cancer Center in Korea between January 2001 and December 2016 were enrolled in the study. The patient data were collected and analyzed retrospectively.
RESULTS: Of the 132 patients, 47 (35.6%) were male, with a median age of 52 years (range, 17 to 81 years). The median follow-up duration was 48.8 months (range, 0.5 to 169.9 months). Helicobacter pylori infection was detected in 82 patients (62.1%). Most patients (80.3%) had stage IE1 according to the modified Ann Arbor staging system. Ninety-two patients underwent bone marrow evaluation, and four patients (4.3%) had marrow involvement. Of these patients, one presented with abdominal lymph node involvement, while the other three had stage IE1 disease if marrow involvement was disregarded. All three patients had no significant symptoms and were monitored after local treatment without evidence of disease aggravation.
CONCLUSIONS: Bone marrow involvement was found in 4.3% of the patients with gastric MALT lymphoma. Bone marrow examination may be deferred because marrow involvement does not change the treatment options or outcome in gastric MALT lymphoma confined to the stomach wall.
Gut Liver 2018 4명 중 한 명 (case 4)는 주변 림프절과 골수 침윤이 있었던 제법 stage가 높은 MALToma였습니다. 비록 골수검사 추적은 되지 못했으나 항암치료 후 10년 이상 생존해 계신다고 합니다.
 9. 환자 설명서 (last update: 2017-2-15)
9. 환자 설명서 (last update: 2017-2-15)
MALT 림프종은 Hp 제균치료 후 호전되기까지 상당한 시간이 필요한 예가 있습니다. 드물게 중간에 악화되어 DLBL 비슷하게 치료 전략을 항암치료로 바꿔야 하는 경우도 있습니다. 일반적인 위암 발생률도 다소 높다고 합니다. 이런 점을 고려하여 환자 설명서를 바꾸었습니다.
MALT 림프종은 위암의 일종이지만 매우 특이한 종류입니다. 분류는 암으로 되어있지만 대부분 (90%) 헬리코박터라는 균과 연관되어 있습니다. 수술은 필요하지 않습니다. 헬리코박터 감염을 가지고 있고 위벽에 국한된 MALT 림프종은 항생제를 이용하여 균만 치료하면 80%에서 림프종이 천천히 사라집니다.
항생제를 이용한 제균치료의 대상인지 확인하기 위하여 몇 가지 검사를 합니다. 검사결과는 약 1주일 후 확인할 수 있습니다. 검사 결과 MALT 림프종이 위벽에만 존재하고 다른 부위에 문제가 없으면 보통 2주 정도의 투약을 합니다. 드물게 약물치료에 반응하지 않으면 방사선치료나 항암치료를 합니다 (20%).
항생제 치료 후 MALT 림프종이 소실되기까지 수개월 혹은 1년 정도 걸립니다. 투약 후 몇 개월 간격으로 내시경과 CT 등을 검사합니다. 중간에 악화되는 소견이 없으면 1년 혹은 1년반까지 기다고 있습니다. 병이 사라지면 (임상적 완전 관해) 1년에 1-2번 정도 검사를 통하여 재발은 없는지, 다른 종류의 위암은 없는지 등을 확인합니다.
 10. 애매한 경우 r/o early stage MALToma 혹은 suggestive (suspicious) of MALToma
10. 애매한 경우 r/o early stage MALToma 혹은 suggestive (suspicious) of MALToma
MALT 림프종의 진단은 digital이라기보다는 analog에 가깝습니다. 애매한 경우는 제균치료 후 경과관찰을 하면 그만입니다. 그러나 산정특례, 암보험 등 의학 외적 문제가 복잡하게 얽혀있는 우리나라에서는 환자에게 설명하는 것이 쉽지 않습니다. 저는 아래와 같이 설명하고 있습니다. 대부분 환자들은 산정특례 및 암보험은 안 되더라도 제균치료에 동의합니다.
애매한 경우입니다. 의학적으로는 애매하지 않은데 돈문제가 애매합니다.
애매하다고 말씀드린 이유는 병리결과지의 "r/o 혹은 suggestive of"라는 용어때문입니다. 이는 "의심되는 정도지 확진은 아니다"입니다. 그런데 간혹 의사에 따라서 암으로 보는 경우도 있습니다. 즉 r/o 이나 suggestive라는 용어의 암여부에 대한 규정이 없기 때문에 병원별, 의사별로 판단이 달라지고 있습니다. 혼란스럽습니다만 표준이 없습니다. 저희는 확진도 아닌데 암으로 진단할 수 없다고 보고 있습니다. 보통의 관점입니다.
위 MALT 림프종은 암으로 분류됩니다. 암에 따른 의료비 경감대상이며, (약관과 보험회사의 정책에 따라 다르지만) 암에 따른 사적보험 급여대상이 될 수도 있고, 헬리코박터 제균치료의 대상이기도 합니다. 암이 아니면 이 모든 것에 해당하지 않습니다. 암이 아니면 의료비 경감대상도 아니고, 사적보험 급여대상도 아닙니다.
과거에는 MALT 림프종 확진이 아니더라도 의심되는 수준이고 헬리코박터가 있으면 치료를 했습니다. 추적관찰에서 MALT 림프종이 안 나오면 "의심단계에서 치료하여 좋아짐. 적절한 단계에서 잘 치료되었음"으로 판단하고 아무 문제 없이 지나갔습니다. 의사는 "암이 되기 전단계에서 치료해서 좋아졌습니다"고 설명하고, 환자는 "미리 치료해서 암이 되지 않았으니 다행이다"고 생각하였습니다. 무척 쉽고 간단했습니다.
그런데 환경이 달라졌습니다. (1) 대한민국 정부는 환자의 진단 코드가 암인지 아닌지에 따라 환자가 내는 돈을 달리하는 정책을 채택하였습니다. 암이면 깎아주는 방향입니다. 좋은 방향입니다. 그러나 애매한 경우가 많아졌습니다. (2) 사적보험에 가입해 있는 환자도 많아졌습니다. 실비 보존 차원이 아니라 암인 경우 수백만원에서 수천만원까지 보험금을 받는 환자가 많아졌습니다.
이 모든 환경 변화는 암인지 아닌지 명확하지 않은 상황에서 환자와 의사의 선택권 축소를 가져왔습니다. 돈문제가 관여되었기 때문입니다. 암을 의심할 수 있는데, 확진이 아닌 경우 치료를 할 수도 없고, 암이 아니라고 말할 수도 없는 어려운 상황에 처하고 마는 것입니다.
지금은 확진이라고 보기 어렵고 (r/o 혹은 suggestive) 헬리코박터 균은 있습니다. 전략은 두가지입니다.
(1) 확진될 때까지 기다림 (=재검). 확진되면 치료. (치료비 경감 혜택이 있거나 보험금을 받을 여지가 있습니다)
(2) 확진이 아니더라도 헬리코박터를 미리 치료. (치료비 경감 혜택은 없고 고액의 보험금을 받는 경우를 보지 못했습니다)돈 문제나 보험 문제를 고려하지 않고 순수하게 의학적으로 판단하면 지금이 헬리코박터 치료 적기입니다. 2주일 투약으로 80%에서 균이 없어집니다. 저의 상황설명에 동의하시면 치료를 시작하겠습니다.
애매한 경우 (내시경 소견 r/o MALToma이지만 조직검사에서 Hp (+), lymphoid follicle로만 나와 의뢰된 환자)에 대하여 외래에서 설명한 기록입니다. 저는 상세히 설명하고 환자의 선택을 존중한다는 입장을 가지고 있습니다. (2017-8-1)
애매한 경우였지만 몇 개월 후 의뢰되어 적절하게 잘 관리되었던 증례입니다.
조직검사에서 H. pylori gastritis with lymphoid follicle 정도의 소견이라도 내시경 육안소견이 MALToma에 합당하면 최종 진단은 거의 항상 MALToma입니다. 현행 심평원 기준과 복잡합 사보험 규정 때문에 H. pylori gastritis with lymphoid follicle 정도의 결과를 받은 상태에서 제균치료를 못하고 추적관찰을 하는 경우가 많은 것 같습니다. 아래 환자가 대표적인 경우입니다. 2013년 12월에 진단을 붙일 수 있었을 것인데, 단지 조직결과가 애매하다는 이유로 몇 개월 늦어졌습니다. 사실 2014년 3월 환자가 제 외래를 찾았을 때 2013년 12월 슬라이드를 빌려서 판독해 보았더니, 본 병원 병리과에서는 MALToma로 진단을 주었습니다. 그래서 저는 최근 애매한 경우는 확진이 안 되더라고 환자에게 자세히 설명하고 암진단이 아닌 상태에서 제균치료를 하는 것을 고려할 수 있도록 기회를 부여하고 있습니다 (EndoTODAY MALToma 조직 진단이 애매한 경우). 여하튼 이 환자는 2014년 3월 진단을 받은 후 제균치료를 받았고 이후는 통상적인 경과를 밟았습니다. 처음에는 rRD로 나왔고, 기다렸더니 pMRD로 바뀌었고, 또 기다렸더니 complete remission으로 호전되었습니다. 내시경 육안 소견도 다소 넓은 전형적인 white atrophic scar였습니다.
검진 조직검사에서 suggestive of early stage of extranodal marginal zone lymphoma of MALT, Hp (+)로 의뢰되었던 중년 남성입니다. MALToma로 진단붙일 것인가, 말 것인가 논란이 가능합니다. 저는 "suggestive of early..."에서는 가능성을 언급할 뿐 확진을 붙이지 않고 있습니다 (K code). 제균치료를 하였고 수 년 간 경과관찰을 하였는데 아무런 문제가 없었습니다. 전문가에 따라서는 MALToma로 확진(C code)하는 것으로 알고 있습니다.
Suggestive of MALToma로 나와 어쩔 수 없이 내시경 재검하였던 증례에 대하여 토론하였습니다. 심평의학, 사법 risk, 보험 risk 때문에 환자 진료와 치료가 상당히 왜곡되고 있습니다.
 11. 위 MALT 림프종 확진 (애매한 경우도 마찬가지입니다) 후 환자를 의뢰할 때에는 제균치료를 하지 말아주시기 바랍니다.
11. 위 MALT 림프종 확진 (애매한 경우도 마찬가지입니다) 후 환자를 의뢰할 때에는 제균치료를 하지 말아주시기 바랍니다.
위 MALT 림프종 확진 (애매한 경우도 마찬가지입니다) 후 환자를 의뢰할 때에는 제균치료를 하지 말아주시기 바랍니다. 환자가 제균치료 약제를 미리 드신 경우는 조직검사 재검을 통한 확진 및 staging workup이 되지 않은 상태에서 치료가 시작된 셈이므로 여러가지 곤란한 상황이 발생합니다. 아래는 대표적인 예입니다.
2014년 환자 의무기록 screenshot
일전에 접수된 외부 병리 슬라이드를 저희 병원에서 재판독한 결과 MALT 림프종 (헬리코박터 균 있음)으로 나왔습니다. 이 질병의 조직학적 진단은 병리의사들 사이에서도 관찰자간 차이가 많습니다. 어떤 분은 의심된다고 판독한 결과를 또 다른 분은 확진으로 판독하는 예가 매우 많습니다. 사실 의심될 때에는 비슷하게 치료하도록 권하고 있는 상황이므로 결과는 마찬가지입니다만... 여하튼 저희는 저희 병리과 판독 결과에 따라 치료방침을 정하고 있습니다. 통상의 경우를 설명하고 환자분에 해당하는 내용을 추가하겠습니다.
+++ 통상의 경우 +++
MALT 림프종은 위암의 일종이지만 매우 특이한 종류입니다. 분류는 암으로 되어있지만 대부분 (90%) 헬리코박터라는 균과 연관되어 있습니다. 수술은 필요하지 않습니다. 헬리코박터 감염을 가지고 있고 위벽에 국한된 MALT 림프종은 항생제를 이용하여 균만 치료하면 80%에서 림프종이 천천히 사라집니다.
항생제를 이용한 제균치료의 대상인지 확인하기 위하여 몇 가지 검사를 합니다. 검사결과는 약 1주일 후 확인할 수 있습니다. 검사 결과 MALT 림프종이 위벽에만 존재하고 다른 부위에 문제가 없으면 보통 2주 정도의 투약을 합니다. 드물게 약물치료에 반응하지 않으면 방사선치료나 항암치료를 합니다 (20%).
항생제 치료 후 MALT 림프종이 소실되기까지 수개월 혹은 1년 정도 걸립니다. 투약 후 몇 개월 간격으로 내시경과 CT 등을 검사합니다. 중간에 악화되는 소견이 없으면 1년 혹은 1년반까지 기다고 있습니다. 병이 사라지면 (임상적 완전 관해) 1년에 1-2번 정도 검사를 통하여 재발은 없는지, 다른 종류의 위암은 없는지 등을 확인합니다.
+++ 환자분의 경우 +++
일단 외부조직검사 슬라이드 재판독 결과 의거 MALT 림프종으로 진단을 붙이겠습니다.
앞서 설명드린 바와 같이 보통 MALT 림프종이 확인되면 병기 결정을 위한 몇 가지 검사 후 위 이외의 다른 장기에 문제가 없으면 헬리코박터 제균치료를 시작하고 있습니다. 그런데 환자분은 이미 헬리코박터 제균치료 약제를 드셨기 때문에 다소 애매해졌습니다. 이런 경우가 아주 많은데요... 저희는 현 단계에서 병기 결정을 위한 기본 검사를 하고 있으며 헬리코박터에 대한 검사와 위 MALT 림프종에 대한 검사는 몇 개월 후에 하고 있습니다. 이미 치료에 필요한 핵심적인 약은 드신 상태이므로 검사 이외에 저희가 추가로 처방할 약제는 없습니다.
몇 개월 후 재검 결과에 따라 아래 세 가지의 시나리오가 가능합니다.
1. 균 (+) --> 균치료 다시 한번 반복
2. 균 (-) 암 (+) --> 기다림
3. 균 (-) 암 (-) --> 가장 좋은 경우입니다. 추적관찰
제발 제균치료를 처방하지 마시고 그냥 의뢰해 주시면 감사하겠습니다.
 12. Collision 또는 MALToma and adenocarcinoma
12. Collision 또는 MALToma and adenocarcinoma
위 MALT lymphoma와 adenocarcinoma 모두 Helicobacter pylori 감염과 관련되어 있습니다. 병인이 같으니 두 병이 동시에 진단되거나 (“Collision tumor”) 혹은 시간 차이를 두고 한 환자에서 진단될 수 있습니다.
60대 여성으로 전정부 MALToma로 진단되고 제균치료로 완전관해에 도달하였습니다. 그런데 4년 후 추적검사에서 우연히 위체하부 대만의 함몰형 위암이 발견되었고 조직검사에서는 poorly differentiated adenocarcinoma가 나왔습니다. 수술을 시행하였습니다.
(2017)
Stomach, subtotal gastrectomy: Early gastric carcinoma
1. Location : middle third, Center at low body and greater curvature
2. Gross type : EGC type IIb+IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size : 1x1 cm
6. Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
7. Resection margin: free from carcinoma, safety margin: proximal 6 cm, distal 10 cm
8. Lymph node metastasis : no metastasis in 33 regional lymph nodes (pN0), (0/33: "1", 0/4; "4sb", 0/0; "5", 0/6; "6", 0/3; "7", 0/4; "8a", 0/0; "9", 0/5; "11p", 0/1; "12a", 0/1; "3", 0/1; "4", 0/6; perigastric, 0/2)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
MALT lymphoma로 제균치료 후 첫 조직검사에서 MALToma와 SRC가 함께 나온 증례도 있었습니다.
(2016) biopsy: signet ring cell carcinoma associated with MALToma (yellow circle)
MALT lymphoma로 제균치료 후 추적관찰 내시경에서 위암이 나와 ESD를 위하여 의뢰되었으나 병소의 경계를 확인할 수 없었고, 재검하여 넓은 위암으로 나와 total gastrectomy를 시행한 증례입니다.
Stomach, radical total gastrectomy: Early gastric carcinoma
1. Location : [1] upper third, [2] middle third, Center at body and circle
2. Gross type : EGC type IIb+IIc
3. Histologic type : extremely well differentiated adenocarcinoma of gastric type
4. Histologic type by Lauren : intestinal
5. Size : 6.0 cm x encircled
6. Depth of invasion : invades submucosa (sm2) (pT1b)
7. Resection margin: free from carcinoma, safety margin: proximal 1.2 cm, distal 16.0 cm
8. Lymph node metastasis : no metastasis in 48 regional lymph nodes (pN0) (0/48: "3,5", 0/12; "4,6", 0/8; "2", 0/2; "5", 0/0; "6", 0/6; "7", 0/5; "9", 0/2; "8a", 0/8; "11p", 0/1; "12a", 0/2; "4sb", 0/0; "1", 0/2; "10", 0/0)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. Associated findings : gastritis cystica profunda
13. AJCC stage by 8th edition: pT1b N0
[2014-7-27. 애독자 질문]
안녕하십니까. EndoTODAY 애독자입니다. MALT lymphoma의 경우 제균치료 후 적절한 f/u biopsy 시기는 언제이고, 제균 치료의 평가는 어떻게 하시는지요? 궤양이 심해 PPI를 유지해야 할 것 같은데 UBT를 하자니 false negative 가능성이 있을 것 같고, 그렇다고 평가를 조기에 안한다면 2차 제균 치료가 늦어질 것 같기도 하구요. 또, 추적시 부분 반응일 경우는 제균치료가 잘 되었다면 언제까지 기다려 보아야 하는 것인지요?
아래 그림처럼 추적 관찰을 한다고 권하셨는데요, 환자가 속쓰림등을 호소하여도 제균 치료 후 PPI는 추가로 처방하지 않습니까? 2주간의 강력한 BID 처방이 있으므로 더 이상 필요하지는 않다고 판단하는 것인지요?
[2014-7-30. 이준행 답변]
좋은 질문 감사합니다. 의학 교과서에는 구체적인 치료방법이 언급되어 있지 않습니다. 가려운 곳을 긁어주지 않는다는 말씀입니다. 실제 환자를 치료하다보면 detail의 중요성을 절감합니다. 문의하신 내용은 모두 detail에 해당합니다. 질높은 진료를 위해서는 detail에 대한 토론이 보다 활성화되어야 할 것 같습니다. EndoTODAY는 detail에 관심이 많습니다. 거대담론에서 빠진 detail 말씀입니다. 하나씩 답해보겠습니다.
1. 적절한 follow up biopsy 시기: MALT 림프종은 빨리 좋아지는 경우도 있지만 천천히 좋아지는 경우도 적지 않습니다.
아산병원의 경험이 요약된 그래프입니다. 어느 병원에서나 비슷합니다. 빨리 좋아지는 사람도 있지만 1년 이후에 좋아지는 환자도 적지 않습니다. 저는 환자에게 이 질병은 원래 좋아져도 천천히 좋아지고, 나빠져도 천천히 나빠지는 병이라고 설명합니다. Follow-up 검사는 조금 천천히 해도 무방하다고 생각합니다. 저의 치료 스케쥴을 소개합니다.
- 0 주: 헬리코박터 제균치료 2주 (Amoxicillin + Clarithromycin + PPI)
- 2 주: 외래진찰. 제균치료 부작용이 없었는지 문진합니다. 특별한 증상이 없으면 아무 투약도 하지 않습니다. 제 경험으로는 적어도 90%에서는 추가 투약이 필요하지 않습니다. 요즘의 MALT 림프종은 대부분 증상이 없는 질병이기 때문입니다. 질병의 경과--좋아져도 천천히, 나빠져도 천천히--를 다시 한번 설명합니다. 8주 후 검사(UBT, EGD, stomach CT, chest PA)를 처방합니다.
- 10 주: UBT, EGD, stomach CT, chest PA. 내시경 육안소견 및 조직검사에서 complete remission이면 6-12개월 후 검사(내시경, stomach CT, chest PA)를 처방합니다. 내시경 육안소견 및 조직검사에서 complete remission이 아니면 3-6개월 후 검사 내시경 검사를 처방합니다. UBT나 조직검사에서 제균이 되지 않았으면 2차 제균요법 1주일을 투약하고 8주 후 UBT 재검을 권합니다.
- 1년 - 1년 반: 육안소견이 악화되지 않는다면 조직검사가 호전되지 않더라도 1년 혹은 1년 반까지 기다립니다. 그래도 호전이 없으면 RT를 추천합니다.
2. 궤양이 심해 PPI를 유지해야 할 것 같은 경우: 사실 MALT 림프종 환자가 궤양이 심해 PPI를 유지해야 할 것 같은 경우는 경험한 적이 없습니다. 설혹 궤양이 작지 않더라도 제균과정에서 2주간의 표준용량 PPI를 아침 저녁으로 먹게 되므로 궤양을 걱정할 필요는 없을 것 같습니다. PPI bid 2주를 포함한 성공적인 제균치료 후에도 여전히 궤양이 문제라면 MALT 림프종이라는 진단을 재검토해야 합니다. MALT 림프종보다는 diffuse large B cell lymphoma 혹은 adenocarcinoma일 것이기 때문입니다.
3. 속쓰림을 호소하는 환자에 대하여: MALT 림프종 환자가 GERD를 함께 가지고 있다면 2주간의 제균치료 후에도 속쓰림은 지속될 것입니다. 그때는 PPI를 투여할 수 있을 것입니다. 그러나 UBT 검사 전에는 잠시 PPI를 끊는 것이 좋습니다. 대부분 가능합니다.
[2015-12-23. 애독자 질문]
외부병원에서 antrum/LC에 nudular lesion 조직검사에서 'lymphoglandular alteration (The possibility of low grade lymphoproliferative lesion (maltoma) 있음), Helicobacter (-)'라고 나왔습니다.
1. 이 환자는 Helicobacter(-) 라도 제균치료를 하는 것이 좋을까요?
2. 만약 재검에서 MALToma 의심소견이 없으도 Helicobacter제균치료를 하는 것이 좋을지요?
3. 위 MALToma는 암중증 등록 하는 것인지요?
4. 위 MALToma는 어떤 코드 넣으시는지요?
[2015-12-26. 이준행 답변]
이 환자는 위점막의 불규칙한 부분이 있으나 MALToma로 진단된 것도 아니고 Helicobacter 감염의 증거도 없었습니다. 따라서 제균치료의 적응증이 아닙니다. 일반 위염에서도 약간의 lymphoepithelial lesion (LEL)이 보일 수 있습니다. 한두 개의 LEL이 있다고 MALToma로 진단하지는 않습니다. 한두 개의 LEL이 있어 병리 선생님이 MALToma 가능성을 언급하였고 Helicobacter가 있다면 (과잉치료라고 비난받을 수 있고, 보험급여도 안되지만) 제균치료를 해 볼 수 있습니다. 그러나 이 환자는 아닙니다.
위 MALToma는 중증등록 대상이며, 과거부터 저는 주로 C88.4를 넣고 있었습니다 (참고).
[2016-1-5. 추가] 그런데 2016년부터 우리나라 코드 체계가 바뀌면서 C85.1을 넣으라는 지침을 받았습니다. 좀 더 알아봐야 할 것 같습니다.
MALT 림프종이 암이라고 생각하십니까?
[2017-1-24. 이준행 답변]
어려운 질문입니다. 왜냐하면 암(cancer)의 정의가 명확하지 않기 때문입니다.
Uncontrolled growth, metastasis를 암의 주된 특징으로 본다면 MALT 림프종의 대부분은 암이라고 부르기 어렵습니다. 아무리 오래 기다려도 uncontrolled growth를 하지 않고 metastasis도 보이지 않기 때문입니다. 그러나 MALT 림프종 중 일부는 분명 uncontrolled growth와 metastasis(골수 침윤이나 림프절 침윤)를 보입니다. 즉 MALT 림프종은 heterogeneous 합니다. 좁은 의미의 암의 특성을 가지고 있는 것도 있지만, 그렇지 않은 종류도 있습니다. 이 둘의 구분이 어렵기 때문에 그냥 전체를 암이라고 부를 수 밖에 없습니다. 아닌 것 같은 것도 아주 많지만 그냥 모두를 암이라고 부릅니다.
암이 잘 정의되어 있는 책은 없는 것 같습니다. 아래 두번째는 제가 본과 2학년 시절에 배운 block 책입니다. 악성 종양과 양성 종양을 나누는 표가 제시되어 있고 악성 종양을 암이라고 정의하고 있습니다. 그런데 문제는 그 중간도 많다는 것입니다. 일부 특성은 암 같고 일부 특성은 암 같지 않은 종류가 있다는 의미입니다. (참고: EndoTODAY 암과 암이 아닌 것으 구분 - 식도 carcinoma in situ에 대하여)
사실 세상은 analog입니다. 암과 암이 아닌 것, 이렇게 두 가지로 명확히 나눌 수 없는 것이 질병의 본질입니다. 암이라고 꼭 나쁜 것도 아니고 암이 아니라고 반드시 좋은 것도 아닙니다. 그냥 편의상 이러이러한 경우를 암이라고 부를 뿐입니다. 암이냐 암이 아니냐를 가지고 장난치는 일부 세력(암보험 등)이 문제인 것이지, 애매한 질병을 애매하다고 말하는 의사가 문제인 것은 아닙니다. (참고: EndoTODAY MALToma 애매한 경우)
요컨데 MALT 림프종이라는 진단에는 암 같은 것과 암 같지 않은 것이 섞여있지만, 정확한 구분은 어렵기 때문에 편의상 모두를 암으로 부르고 있는 것 아닌가 생각됩니다. (참고: EndoTODAY MALToma)
[2017-1-24. 서울대 특강 질문]
10년 후에도 MALT 림프종이라는 진단명이 살아남을 것 같습니까?
[2017-1-24. 이준행 답변]
혹시 세분화되어 일부는 빠지고 일부는 남게될지 모르겠습니다만, 완전히 사라질 것 같지는 않습니다.
[2017-1-24. 서울대 특강 질문]
Helicobacter negative MALToma는 어떻게 하고 계시는지요?
[2017-1-24. 이준행 답변]
저는 Helicobacter 음성 MALT 림프종이라고 판단된 경우라도 일단 제균치료를 시행한 후 경과관찰을 합니다. 영 호전이 없으면 RT를 권합니다. 최근에는 꼭 H. pylori serology를 하고 있습니다. Serology까지 음성이어야만 진정한 H. pylori 음성 MALToma 아닌가 생각하고 있습니다. (참고: EndoTODAY Hp 음성 MALToma)
MALT lymphoma가 gastric DLBCL (diffuse large B cell lymphoma)로 바뀐다고 생각하십니까? 다른 말로 diffuse large B cell lymphoma of the stomach이 MALT lymphoma에서 시작하는 것으로 보시는지요?
[2017-1-24. 이준행 답변]
저는 1997년부터 2000년 4월까지 군대에 다녀왔습니다. 제가 군대에 가기 전 MALT lymphoma는 분명히 (1) high grade component가 있는 경우(Regression of gastric high grade MALT lymphoma after H. pylori eradication. Montalban C. Gut 2001)와 (2) high grade component가 없는 경우로 나뉘었습니다.
그런데 제가 군대에 다녀온 후 살펴보니 MALToma의 범위가 (1) high grade component가 없는 경우로 축소되어 있었습니다. 어떻게 이렇게 변했는지 trace는 어려웠습니다. 그냥 병리의사들이 얼렁뚱땅 바꾼 것 아닌가 추정하고 있습니다.
저는 전부는 아닐지 몰라도 대부분의 위 림프종은 MALT 조직에서 발생하는 것 아닌가 추정하고 있습니다. 일부는 일정 기간의 low grade MALToma 기간을 거쳐서 DLBCL이 되겠지만, 더 많은 경우는 low grade MALToma 기간을 아주 짧게 거치거나 혹은 아예 거치지 않고 DLBCL이 될 것 같습니다. 그래도 세포의 기원은 MALT 조직일 것으로 짐작합니다.
[2017-1-24. 서울대 특강 질문]
Colon MALToma 등 extraintestinal MALT lymphoma에 대해서는 어떻게 하고 계시는지요?
[2017-1-24. 이준행 답변]
증례가 많지 않고 제가 진료하는 분야가 아니라서 정확히 답변드리기 어렵습니다. 일단 H. pylori 제균치료를 해 보기도 하고 (Kelley SR. Int J Colorectal Dis 2016), RT를 하기도 합니다. 최근에는 flat adenoma로 생각하고 EMR을 한 환자에서 colon MALToma가 나온 경우가 있는게 그냥 경과관찰 하고 있습니다. 아래에 옮깁니다.
외부 내시경에서 cecum에 0.8cm의 flat elevated lesion으로 의뢰됨. 조직검사나 용종절제술은 시행되지 않은 상태였음.
병리결과 "dense infiltration of small lymphocytes with lymphoid follicle formation and multifocal lymphoepithelial lesions, suggestive of extranodal marginal zone lymphoa of MALT"였음. Staging workup에서 다른 부위 lymphoma는 없었음. 추가 치료 없이 6개월 후 추적내시경을 하였고 특이 소견이 없었음.
* 참고: EndoTODAY Extragastric MALToma
교수님 안녕하십니까. 지난 화요일 오전 강의들었던 분당서울대학교병원 임상강사입니다.
강의 후 올려주신 자료를 보다가 궁금한 것이 있어 문의드리려고 메일 드립니다.
1) 저는 EUS 등으로 stage IE1 (점막이나 점막하층에 국한)과 stage IE2 (근육층 이상 침범)를 확인하여 IE1에서만 H. pylori 제균치료를 하는 것으로 알고 있었습니다. 그런데 선생님 강의자료를 보면 stage IE에서도 H. pylori 제균치료를 하는 것으로 되어 있습니다 (아래 그림).
지난번 강의 때 말씀하셨던 것처럼 (1) EUS를 하더라도 사실상 IE1과 IE2의 구분이 쉽지 않고, (2) H. pylori 제균치료가 쉽기 때문에 IE1과 IE2를 나누지 않고 우선 제균치료를 시도하는 것이 좋겠다는 의미인지요? 혹시 치료 가이드라인이 바뀐 것인지 궁금합니다.
[2017-1-27. 이준행 답변]
좋은 질문입니다. 1월 24일 강의 자료를 다시 살펴보았습니다. 제가 personal protocol이라고 보여드린 아래 슬라이드가 약간의 혼선을 일으킬 수 있겠다고 느꼈습니다. Stage IE2에 'HPE or ChemoRx'로 되어 있지만 사실 저는 stage IE2의 첫 치료로 대부분 HPE를 선택하고 있습니다.
각 병원의 많은 전문가들도 저와 같은 방식을 선택하고 있습니다. 선생님께서 지적하신 슬라이드, 즉 stage IE에서는 IE1과 IE2를 나누지 않고 모두 제균치료를 하는 diagram은 서울대병원의 자료입니다 (Chung SJ. J Clin Gastroenterol 2009). 최근 발표된 서울아산병원 자료를 보더라도 IE2에서도 초치료는 대부분 제균치료를 선택하고 있습니다 (Gong EJ. Gut Liver 2016). Stage IE2라고 하더라도 매우 큰 mass를 형성하고 있는 경우만 아니라면 H. pylori 제균치료를 하고 조금 지켜본 후 추가치료 여부를 결정해도 늦지 않을 것으로 생각됩니다. 이런 이유로 EndoTODAY MALToma 치료부분에는 아래와 같은 두 개의 algorithm을 소개하고 있습니다.
MALT 림프종의 치료에 대하여 널리 인정받는 치료 가이드라인은 없습니다. ESMO (European Society for Medical Oncology)에서 2013년 제시한 가이드라인이 드물게 인용될 뿐입니다 (Zucca. Ann Oncol 2013 - free PDF). ESMO 2013년 가이드라인은 조금 더 놀랍습니다. 위벽에 국한된 stage IE에서는 depth of invasion을 고려하지 않고 H. pylori 제균치료를 하도록 권하고 있습니다. 심지어는 intra-abdominal node가 있는 stage IIE에서도 H. pylori 제균치료를 권하고 있을 정도입니다.
실제 현장에서는 임상의사들의 경험과 preference가 상당히 중요한 것 같습니다. 왜냐구요? (1) 암으로 분류되었는데 항생제만 쓴다는 것이 늘 걱정스럽기 때문이고, (2) 강한 치료가 있는데 약한 치료만 한다는 것이 마음에 걸리기 때문이고, (3) 병이 있는데도 치료하지 않고 기다린다는 것도 의사나 환자 모두에게 상당히 어려운 일이기 때문입니다. 원래 위 MALT 림프종은 인내심을 가지고 천천히 천천히 치료해도 좋은 병이며, 심지어는 잔류병소가 있거나 stage IV에서도 asymptomatic하면 'wait and see'를 선택할 수 있습니다 (EMSO 2013 diagram). 단지 우리나라 의료 현장에서 이를 적용하기 어려울 뿐입니다. 다들 급하니까. 성격이 급한 의사를 만나면 많은 검사와 빠르고 강한 치료를 받게 되고, 느긋한 성격의 의사를 만나면 최소한의 검사와 느리고 약한 치료를 받게 되는 것이 위 MALT 림프종 환자의 처지입니다. 운 혹은 운명같은 것이지요. 다행스럽게 환자 경험이 많은 전문가들 사이에서 자연스러운 암묵적 합의가 이루어지면서 점차 최소한의 검사와 느리고 약한 치료로 방향이 잡히고 있습니다.
2017년 2월 대한소화기내시경학회 증례 (헬리코박터 제균 치료 후 재발된 위 점막연관림프조직 림프종) 저자이신 김경오 교수님께 질문을 드립니다.
제가 이해하기로는 MALT 림프종 재발예를 모두 급히 서둘러 치료할 필요는 없는 것 같습니다. Wait and see를 권하는 기관도 있을 정도입니다. EMSO 2013년 가이드라인 (Zucca. Ann Oncol 2013)에는 다음과 같이 언급되어 있습니다. "In the case of persistent but stable residual
disease or histological relapse (without distant dissemination and/or gross endoscopic tumour), a watch-and-wait policy appears to be safe".
선생님의 재발예는 즉시 방사선 치료를 하셨던데요..... 어떤 경우는 즉시 치료를 하고 어떤 경우는 wait and see를 할 수 있겠는지 선생님의 의견을 듣고 싶습니다.
[2017-2-12. 김경오 교수님 답변]
이번 교육자료에 대해 관심을 갖고 고견을 주셔서 감사합니다. 선생님 말씀대로 완전 관해 후 재발 예에 대해 반드시 즉시 방사선 치료를 해야 할 필요는 없다고 생각합니다. 2017년 NCCN 가이드라인에는 완전 관해 후 재발한 경우 헬리코박터 양성이고 무증상 stable state인 경우 2차 제균치료를
권고하고 있고 헬리코박터 음성인 경우 3개월 후 추적검사 또는 방사선 치료를 할 수 있다고 되어 있습니다. 두 가지 모두 선택 가능한 옵션으로 권고되고 있으므로 그때 그때 상황에 따라 선택할 수 밖에 없을 것으로 보입니다. 저는 환자가 추적관찰만 하는 것을 불안해 할 경우 방사선 치료를 권고하고 그렇지 않으면 2~3개월 후 추적 검사를 권고하고 있습니다. 이번 교육자료에 실린 증례도 재발 확인 후 3개월 후 다시 조직검사를 시행하였고 역시 MALT lymphoma로 진단되었기에 방사선 치료를 시행하였습니다.
[2017-2-13. 애독자 질문]
안녕하세요 교수님. 내시경 육안소견에서 MALToma를 의심하지는 않았으나 single erosion 혹은 single erythematous lesion 조직검사에서 prominent lymphoid hyperplasia, H. pylori (+)로 나오는 경우 어떻게 대처해야 할 지 문의드립니다. 2개월후 추적내시경에서 병변이 사라졌더라도 조직검사 재검이 필요한지, 조직검사 재검에서 같은 조직 소견이 나오면 제균을 권해야 하는지 의문입니다.
[2017-2-13. 이준행 답변]
우리나라에서 Helicobacter 제균치료 적응증이 너무 tight해서 생기는 문제입니다. 일본에서는 내시경 소견과 무관하게 Helicobacter pylori가 있으면 제균치료를 하도록 권하고 있는데, 제 마음 속으로는 일본 방식이 좋다고 생각합니다. 일본 같으면 당연히 제균치료를 하는 상황이라는 말씀입니다.
심평원의 삭감 위협이 상존하는 우리나라에서는 의사의 선택권이 크게 제한받고 있습니다. 치료를 하고 싶어도 못하는 경우가 너무 많다는 것입니다. 문의하신 것처럼 prominent lymphoid hyperplasia로 나온 사람 중 추적 내시경에서 MALToma로 확진된 경우가 종종 있습니다. 따라서 (비록 규정 위반이고 삭감 우려가 있지만) 제균치료를 하는 것이 좋겠다고 생각합니다. 추적 내시경에서 병소가 없으면 구태여 조직검사까지는 필요하지 않을 것 같습니다.
50대 초반 남성입니다. 건진 내시경에서 작은 궤양이 발견되었고 조직검사에서 암 소견이 없어서 양성위궤양으로 판단하여 1주간의 헬리코박터 제균치료 + 3주간의 PPI 투약 후 추적내시경 검사를 시행하였습니다. 다소 이상한 모양의 궤양 반흔이었는데 조직검사에서 MALToma가 나왔습니다. 어떻게 해야 좋을지 문의드립니다.
[2017-4-28. 이준행 답변]
MALT 림프종인데 첫 진단에서 underestimation 된 경우로 판단됩니다. 첫 내시경 사진을 보면 작고 얕은 궤양은 있지만 fold는 궤양 경계와 약간 떨어진 곳에서 멈추고 있습니다. 궤양과 fold 끝 사이에도 점막병소가 있다는 의미이고, 실제로 약간의 발적과 표면 변화가 있습니다. 후향적으로 판단하면 양성 위궤양은 아니었습니다. 병리 슬라이드를 리뷰하면 좋겠습니다. 병리 선생님께서 특별히 chronic gastritis, active, with lymphoid follicles라고 언급한 것도 뭔가 의미가 있었을 것 같습니다.
추적내시경 사진도 예쁘게 아문 궤양 반흔이 아니고, MALT 림프종 치료 후 관찰되는 white atrophic scar에 합당한 모양입니다. 그러니까 처음부터 MALT 림프종이었던 것으로 보면 무난합니다.
일단 제균치료는 하였고 육안적으로 호전되었는데, 단지 조직검사에서 MALT 림프종이 나오고 있으므로 지금은 기다리면 됩니다. (어쩔 수 없는 사연으로 약간 늦었지만) Stomach CT 정도 찍어서 주변 림프절에는 문제가 없는지 확인해 두는 정도가 전부일 것 같습니다. 3-6개월 간격으로 내시경 및 조직검사를 하여 완전 관해가 오는지 확인하면 되겠고 1년이나 1년 반 후까지 완전 관해가 오지 않으면 방사선 치료를 고려하면 어떻겠습니까?
[2017-8-29. 애독자 질문]
현재 근무하는 병원 교수님 말씀 및 EndoTODAY에 교수님께서 쓰신 내용을 보면 HPE기간이 2주라고 알고 있습니다. 하지만, 지난 주말 킨텍스 소화기내시경학회 세미나에서 발표하신 연자께서는 initial treatment 로 eradication 기간을 1주로 하신다고하여 혼동스러웠습니다. NCCN guideline에보면 기간은 따로 명시하지 않고, “Currently accepted antibiotic therapy for H. pylori” 이렇게만 되어있습니다.
HPE 2주 투여가, 더 높은 제균율을 기대하여 그렇게 하시는 것으로 생각되는데, 혹시 다른 이유라던지, 특별한 근거가 있으신지 답변 부탁드립니다.
[2017-8-29. 이준행 답변]
물론 2주 제균율이 조금 더 좋습니다. 아주 조금.... 거의 무시해도 좋을 정도로 조금. 그래서 다른 교수님이 1주라고 하신 것도 타당한 처방입니다.
그러나 저는 다른 요소도 봅니다. 제균치료 기간을 제균율만으로 결정하지 않습니다. 환자의 compliance도 고려합니다. 1주 치료는 암 치료로서는 너무 짧은지라 치료한 것 같은 느낌, 감(感), 기분 같은 것이 들지 않습니다. 환자에게 말입니다. 저는 이런 점도 중요하게 다룹니다. 그래서 2주 입니다.
선생님이 만나는 환자들이 어떠한지를 잘 보고 적절히 조절하는 것도 필요한 일입니다. 유명한 의사가 되는 길은 아니지만... 인자한 의사가 되는 길이 될 것입니다. 환자의 마음도 살피는 것이지요.
의뢰드린 MALToma 환자에 대한 질문입니다.
(1) 확진 후 제균치료 3제 요법 14일 처방을 받은 것을 압니다. 이 경우 제균치료 7일 초과한 부분은 삭감은 안되는지요?
(2) PPI는 rabeprazole을 선택하셨던데, 제가 알기론 rabeprazole이 Tmax 도달시간이 빨라 다른 PPI보다 약효가 더 빨리 나온다고 알고 있습니다. 위장내시경학회에서 얼핏 들은 기억으론 rabeprazole이 상대적으로 좀더 낮은 pH에서도 약효 발현이 잘되서 좀더 빠른 증상호전을 기대해볼수 있다고 했던 기억도 납니다. 예전에 교수님께 제가 제균치료시 PPI별로 제균성공률에 차이가 있냐고 문의드렸을때 omeprazole만 아니면 나머지 PPi들은 별차이가 없다고 들었던 기억이 있습니다. 교수님께서 rabeprazole을 선택하신 이유는 그래도 Tmax가 빠르니까 조금이라도 제균성공률이 더 높을 것이란 기대감에서 선택하신건지요. 사실 저두 상기 이유, 기대감으로 작년말부터 저희쪽 3제요법 약속처방에 rabeprazole제균치료 묶음을 등록해두고 저두 rabeprazole을 사용 중입니다. SMC는 rabeprazole이 라비에트정만 등록되어 있나요? 오리지널은 파리에트인데....아주대 교수님들도 제균치료시 PPI를 rabeprazole로 하실땐 라비에트정으로 하시더라구요. 라비에트가 일동제약인가로 알고 있는데, 전에 제약사 부스에서 라비에트가 다른 rabeprazole보다도 Tmax가 좀더 빨리 도달해서효과가 좀더 빠르다고 광고하던데...오리지널인 파리에트와 생동성 시험 통과했다는데 Tmax가 오리지널보다 더 빠르다고 하니...그럼 약효도 더 빨리 사라질것 같은데... 그런 생각들을 했었던 기억이 납니다. Rabeprazole, 그 중에서도 라비에트정을 선택하신 이유가 궁금해서 여쭤봅니다.
(3) 의뢰드린 환자의 경우 staging w/u CT에서 "a few prominent lymph nodes in left gastric area"라고 판독되어 있던데요, MALToma에서 이런 경우 LN Bx를 할 수 없는 상황인데, 이 정도로도 LN 침범으로 보는건가요? 아니면 그냥 H. pylori-associated gastritis환자들 CT에서 prominent LN 보이는 것처럼 LN metastasis가 아닌, reactive change정도로 보시는지요. 금년 상반기에 이혁 교수님께 의뢰드렸던 제 환자가 이런 케이스가 있었는데, AGC B-IV일까 싶어서 (위벽도 두꺼워져있어서) 걱정했는데 제균치료후에 CT f/u하니까 호전된 경우를 경험한바 있었습니다. MALToma확진되면 staing w/u은 하지만, 제 환자들 중 MALToma로 CT찍어서 prominent LN가 나온 경우가 거의 없었던 것 같아서 어떻게 해석하는지 궁금합니다.
[2017-10-1. 이준행 답변]
1) 제균치료 기간을 1주일로 할 것인가 2주로 할 것인가는 2017년 내시경학회 세미나 후 한 애독자께서 주신 질문과 저의 답변을 참고하시기 바랍니다. 아래에 옮깁니다. MALT 림프종 환자에서 제균치료 기간을 2주로 잡았다는 이유로 삭감은 하는 경우는 별로 없는 것 같습니다. 지역마다 평가 기준에 일관성이 없다고 알려져 있기는 하지만... 암환자에게 몇 천원짜리 약 1주일 드리는 것 때문에 걱정을 해야하는 우리나라 현실이 한심하기 그지 없습니다.
물론 2주 제균율이 조금 더 좋습니다. 아주 조금.... 거의 무시해도 좋을 정도로 조금. 그래서 다른 교수님이 1주라고 하신 것도 타당한 처방입니다. 그러나 저는 다른 요소도 봅니다. 제균치료 기간을 제균율만으로 결정하지 않습니다. 환자의 compliance도 고려합니다. 1주 치료는 암 치료로서는 너무 짧은지라 치료한 것 같은 느낌, 감(感), 기분 같은 것이 들지 않습니다. 환자에게 말입니다. 저는 이런 점도 중요하게 다룹니다. 그래서 2주 입니다. 선생님이 만나는 환자들이 어떠한지를 잘 보고 적절히 조절하는 것도 필요한 일입니다. 유명한 의사가 되는 길은 아니지만... 인자한 의사가 되는 길이 될 것입니다. 환자의 마음도 살피는 것이지요.
2) 제균치료의 성공률에 PPI의 종류가 미치는 영향은 크지 않습니다. PPI의 종류에 따른 제균율 차이에 대한 head-to-head comparison 연구는 거의 없습니다. 일단 모두 비슷하다고 봐도 무방할 것 같습니다. 회사마다 자기 제품이 더 좋다는 이런 저런 이유를 홍보합니다. Rabeprazole의 경우는 Tmax 도달시간이 어떻고 작용시간이 어떻고 이야기를 합니다. 그러나 다른 회사에서는 또 다른 이유를 들어 자기 회사 제품이 더 좋다고 이야기합니다. A 회사 sponsor 연구는 A 제품이 좋다는 결론이고 B 회사 sponsor 연구는 B 제품이 좋다는 결론이니 믿을 것이 없습니다. 여러 회사의 제품을 direct하게 비교한 연구는 거의 없는 실정입니다. 그래서 제가 내린 개인적 결론은 'GERD 증상 조절이나 H. pylori 제균치료에 있어서 (omeprazole을 제외한) PPI의 효과는 약제 사이에 거의 차이가 없다'는 것입니다. 제가 1차 제균치료에 rabeprazole을 쓰는 것은 특별한 이유가 없습니다. 어쩌다보니 그리 된 것입니다. 제가 발령받은 지 얼마 되지 않았을 때 작은 임상연구가 있었는데, 그때 rabeprazole을 쓰게 되었습니다. 지금까지 바꿔야 할 특별한 이유를 찾지 못하여 그냥 그대로 쓰고 있을 뿐입니다. Tmax를 고려하거나 작용시간을 고려한 것은 절대 아닙니다. 완전히 우연한 결과입니다. 그냥 어쩌다 쓰게 되었는데 별로 나쁘지 않아서 그대로 가는 것일 뿐입니다.
저희 병원에서는 ESD 후 PPI로 lansoprazole을 쓰고 있습니다. CP에 박혀 있어서 다른 약을 쓰기 어렵습니다 (CP에 어떤 약을 쓴다는 것은 무서운 일입니다. 한번 CP에 들어가면 바꾸기 어렵습니다. 선택된 회사 입장에서는 CP에 따른 처방이 계속 발생하니 그야말로 '누워서 떡먹기'지만... 다른 회사의 입장에서는 어처구니 없는 일이지요. 뚫고 들어갈 방법이 없으니까요. CP를 만들 때 몇 년에 한번 바꾼다는 것을 미리 정해야 할 것 같습니다. 저희도 경험이 없어서 그렇게 design 하지 못했지만... ). 그래서 저는 일반적인 GERD나 H. pylori 제균치료에는 lansoprazole이 아닌 다른 약을 쓰고 있습니다. 여러 회사의 PPI를 전체적으로 비슷하게 사용하려다보니 그리 되었습니다. 다 비슷하니까 어떤 약 하나를 특별히 많이 처방할 이유가 없습니다. 괜히 의심 받습니다. 과거 어떤 교수님이 월요일은 esomeprazole, 화요일은 rabeprazole, 수요일은 pantoprazole과 같이 처방하여 균형을 잡고 있다고 들었는데 좋은 방법이라고 생각합니다. 짝수 날, 홀수 날 나눠 쓰는 분도 계십니다. 병록번호 끝자리에 따라 달리 쓰는 분도 계십니다. 여하튼 여러 PPI가 다 비슷합니다. 한마디로 다 좋습니다. 더 좋은 것이 없습니다. 아무 것이나 써도 됩니다. (한 약제에 부작용이 있을 때 다른 약으로 바꾸는 경우는 있습니다.)
제가 라비에트를 쓰는지 어떤 약을 쓰는지 저도 잘 모릅니다. 성분처방을 하니까요. 대형 병원에서는 어느 날 갑자기 상품명이 바뀌기도 합니다. 공개 입찰 때문이지요. 저는 original 약을 좋아하는 편이었는데, 공정성을 중요시하는 우리나라의 제도가 original만 쓰는 것을 곱게 보지 않는다는 것을 알아버렸습니다. 사실 모든 의사가 original만 고집하면 외국계 대형 제약회사만 살고 국내 제약사는 다 죽으라는 말이나 다름 없습니다. 여하튼 저는 성분처방을 합니다. Original이 되기도 하고 아니기도 합니다. 제 손을 떠난 이슈입니다.
3) MALToma의 초치료 대상을 어떻게 설정할 것인가의 이슈입니다. 물론 proper muscle invasion이 있거나 림프절 전이가 있으면 제균치료의 효과가 떨어질 것 같습니다. 그러나 proper muscle invasion이 있거나 림프절 전이를 정확히 평가할 방법이 없습니다. 반면 제균치료는 무척 간단합니다. 그래서 최근에는 proper muscle invasion 혹은 림프절 전이가 약간 의심되더라도 일단 제균치료 후 경과관찰을 하는 경향입니다. 정말 심하고 뚜렷한 전이가 없으면 제균치료를 해 볼 수 있다는 것입니다.
MALT 림프종의 치료에 대하여 널리 인정받는 치료 가이드라인은 없지만 ESMO (European Society for Medical Oncology)에서 2013년 제시한 가이드라인을 참고하는 분이 많습니다 (Zucca. Ann Oncol 2013). 이에 따르면 위벽에 국한된 stage IE에서는 depth of invasion을 고려하지 않고 H. pylori 제균치료를 하도록 되어 있습니다. 심지어는 intra-abdominal node가 있는 stage IIE에서도 H. pylori 제균치료를 권하고 있을 정도입니다.
어짜피 정확할 수 없는 clinicial staging을 위하여 환자를 고생시키기보다는 minimal한 검사 후 제균치료를 하고 이후에 잘 follow-up 하는 것이 현실적인 방법이라고 생각합니다. 저는 그렇게 하고 있습니다. 그런 이유로 EUS도 잘 하지 않고 골수 검사도 잘 하지 않습니다. 사실 거의 하지 않습니다.
답변이 되었기 바랍니다.
마침, 평소에 고민이 많았던 증례를 언급해주셔서 반가운 마음에 댓글을 올립니다 (EndoTODAY 위암 546). Suggestive of MALToma. 항상 고민이 많은 질병인것 같습니다. 안타깝게도 제 경험상 한번에 진단이 되는 경우가 거의 없었습니다.^^;; Wotherspoon grade 3~4 소견이 있으나, IgH rearrangement에서 monoclonality 보이지 않는 경우 보통 교수님께서는 재검을 하시는지요? 교수님 글에서는 애매한 경우 제균치료를 우선적으로 해볼 수 있도록 권유를 한다고 되어 있긴 한데.. 혹시나 f/u 검사에서 호전이 없어 방사선 치료 등이 필요한 소견으로 나오게 된다면 진단없이 치료를 할 수 있는가 궁금하기도 하구요.. 확진 되지 않고 제균 치료를 하는 경우 진단코드는 어떻게 부여를 하시는지, EUS 나 복부 CT 등 w/u 은 어떻게 진행하시는지 교수님 고견이 궁금합니다 ^^
[2017-11-14. 이준행 답변]
EndoTODAY MALToma 애매한 경우에 소개한 바 있지만 오늘은 조금 더 자세한 질문이 있어서 제 의견을 드립니다. 답은 아닙니다. 의견입니다.
[질문 1] 안타깝게도 제 경험상 한번에 진단이 되는 경우가 거의 없었습니다.^^;;
[답변 1] 병리과 선생님에 따른 차이가 큽니다. 본 병원 병리과에도 위 조직검사를 봐주시는 병리과 선생님이 여럿 계시는데, 선생님별로 MALToma 진단 눈높이는 제법 다릅니다. Lymphoma 전문가 선생님께서 MALToma 진단을 가장 잘 붙여주십니다. Lymphoma 전문가가 아닌 선생님들은 자꾸 유보적인 진단을 주십니다. r/o, suggestive of, suspicious of, atypical lymphoid cells, single lymphoepithelial lesion (LEL) 등등... 그래서 내시경 소견 상 MALToma가 틀림없다고 생각되면 조직검사 슬라이드를 lymphoma 전문가 선생님께서 봐 달라고 따로 부탁하고 있습니다.
[질문 2] Wotherspoon grade 3~4 소견이 있으나, IgH rearrangement에서 monoclonality 보이지 않는 경우 보통 교수님께서는 재검을 하시는지요?
[답변 2] 저희는 Wotherspoon grade를 잘 사용하지 않아서 개인적 경험은 적습니다. IgH rearrangement의 monoclonality 여부에 따라 MALToma 진단을 붙이기는 어렵습니다. 그래서 별로 의미 부여를 하지 않습니다. 저는 내시경 사진을 뚫어지게 바라보고, 조직검사 결과를 어떤 병리과 선생님이 sign을 하신 것인지 잘 살펴봅니다. 그리고 병리과 선생님을 찾아가 토론을 합니다. 재검은 병리과 선생님과 토론 및 협의가 된 이후에 시행합니다. 애매한 상태에서 여러번 조직검사를 한다고 답이 나온다고 생각치 않습니다.
[질문 3] 애매한 경우 제균치료를 우선적으로 해볼 수 있도록 권유를 한다고 되어 있긴 한데.. 혹시나 f/u 검사에서 호전이 없어 방사선 치료 등이 필요한 소견으로 나오게 된다면 진단없이 치료를 할 수 있는가 궁금하기도 하구요.
[답변 3] 애매한 경우 제균치료를 한 환자에서 나중에 문제된 경우는 없었습니다. 육안소견이 매우 경미하고 조직검사에서 애매하게 나온 경우만 제균치료를 하고 있기 때문입니다. 제법 뚜렷한 종양이나 궤양을 형성한 MALToma 의심병소인데 조직검사가 애매한 경우는 치료에 들어가지 않고 어떻게든 확진을 붙이기 위하여 노력하고 있습니다. 만약 애매한 경우에 제균치료를 하였는데 나중에 뚜렷한 병이 진단된다면.... 그런 경우는 없었지만... 만약 만나게 된다면 "MALToma로 진행하는 것을 예방하기 위하여 최대한 힘썼지만, 우리의 노력에도 불구하고 결국 MALToma가 되고 말았습니다. 아쉽지만... 현 상태에서 최선의 방안을 찾아봅시다."라고 말할 것 같습니다. 그게 사실이니까.
[질문 4] 확진되지 않고 제균 치료를 하는 경우 진단코드는 어떻게 부여하시는지, EUS 나 복부 CT 등 w/u 은 어떻게 진행하시는지 교수님 고견이 궁금합니다 ^^
[답변 4] 헬리코박터 위염에 준하여 K29.7 코드로 치료하고 있습니다. EUS는 하지 않고 있습니다. EUS는 MALToma에서도 하지 않는데 애매한 경우에는 더욱 할 필요가 없다고 생각합니다. CT는 MALToma에서는 늘 시행합니다. 애매한 경우는 거의 하지 않고 있지만, 뭔가 감이 안 좋아 몇 번 했던 적이 있는 것 같습니다.
EndoTODAY MALToma 애매한 경우를 참고하시기 바랍니다.
1. MALToma 환자의 CT에서 left gastric area의 indeterminate lymph node가 보이는 경우가 있습니다.
2. LN 침범 (또는 BM 침범) 이었다하더라도 HpE 후 내시경적 호전을 보인다면 CR을 기대하면서 언제까지 기다려볼 수 있을까라는 고민도 들었습니다. 혹여 BM 침범이었다면 HpE 후 내시경적 관해가 온다면 BM Bx를 f/u 하여 BM 호전까지 확인해야하나라는 생각도 들었구요
3. MALToma의 병기가 무척이나 헷갈렸습니다. Lugano system 에는 III라는 병기가 없어서 몇번씩 잘못봤나 쳐다봤었습니다. 그리고 II'E'의 E의 의미가 Ann Arbor system에서의 E(Extralymphnodal)의 의미와 달라서 무척이나 낯설게 느껴져서 머리에 잘 들어오지가 않았습니다. Modified Ann Arbor system 분류가 제일 이해가 쉽고 깔끔해보입니다. 학회나 공식적인 논문에서 어떤 staging system으로 언급하는지에 따라 의사소통이 달라질 것 같은 생각이 드는데 어떤 분류가 널리 쓰이는 것인지 궁금합니다.
4. 만약 향후 local에서 MALToma 를 발견하게 된다면, local에서 치료를 시도해봐도 될지, HPE하고도 기다려보다가 불안하거나, 호전이 없거나하여 3차병원에 의뢰한 경우, 3차병원에서도 치료 plan을 정하는데에 혼선이 생길 것 같아 바로 보내는 것이 맞은 것 같기도 합니다. 교수님 의견은 어떠신지요?
[2017-11-28. 이준행 답변]
1. CT에서 보이는 작은 left gastric node는 워낙 nonspecific한 것이 많아서 나중에 문제되기 전까지는 그냥 크게 고려하지 않으셔도 좋을 것 같습니다. 제균치료하고 오래 보다가 진행했다 싶으면 그 때 종양내과와 상의하여 CHOP을 시도하면 반응이 매우 좋습니다. 너무 걱정하지 말고 대담하게 접근하는 편이 환자에게 유리할 것 같습니다.
2. Bone marrow involvement가 있어도 제균치료를 하면 좋아지는 경우도 있습니다. 저는 단 한명 있었는데 그 환자는 10년 넘었는데 아직 잘 살고 있습니다. 관련하여 아산병원의 논문이 있고 민병훈 선생님의 논문이 있습니다.
3. 사실 소화기내과 의사 입장에서 MALToma는 staging을 따지고 말 것도 없습니다. Oncologist 입장에서는 매우 이상한 일이지만 MALToma에서는 staging 자체가 별로 의미가 없어서 (예를 들면 BM involvement가 있으면 stage IV인데 잘 사시거든요) 그냥 논문쓸 때 한번 정리하면 됩니다. Staging에 따라 치료방침 정하는 그런 것 아닙니다. 그냥 종양이 큰지, 근육층 침범이 있는지, definite한 metastasis가 있는지 정도를 확인하고 없으면 제균치료를 하면 됩니다. Staging을 한다면 Ann Arbor를 약간 변형해서 사용하는 것이 보통입니다 (참고).
4. Local에서는 치료하지 않는 것이 좋습니다. 이유는 많아요.
1) 한 명의 병리의사가 계속 봐야 하는데, 환자의 병리 슬라이드를 누가 보도록 지정하기가 어렵습니다. 보통 계속 바뀝니다. 병리 의사들과 빨리 연락되지 않는 경우도 많습니다.
그래서 개업가에서는 MALToma 나오면 바로 보내는 것이 상책입니다. 잘 된 경우만 보고 그냥 개업가에서 치료하다보면 곤란한 상황에 빠지기 쉽습니다.
[2020-8-6. 이혁 교수님 특강]
다양한 morphology를 보이지만 elevated type이 Hp 제균치료에 대한 반응이 떨어집니다.
Mapping biopsy는 서구에서 권유되지만 우리나라에서는 별 의미는 없습니다.
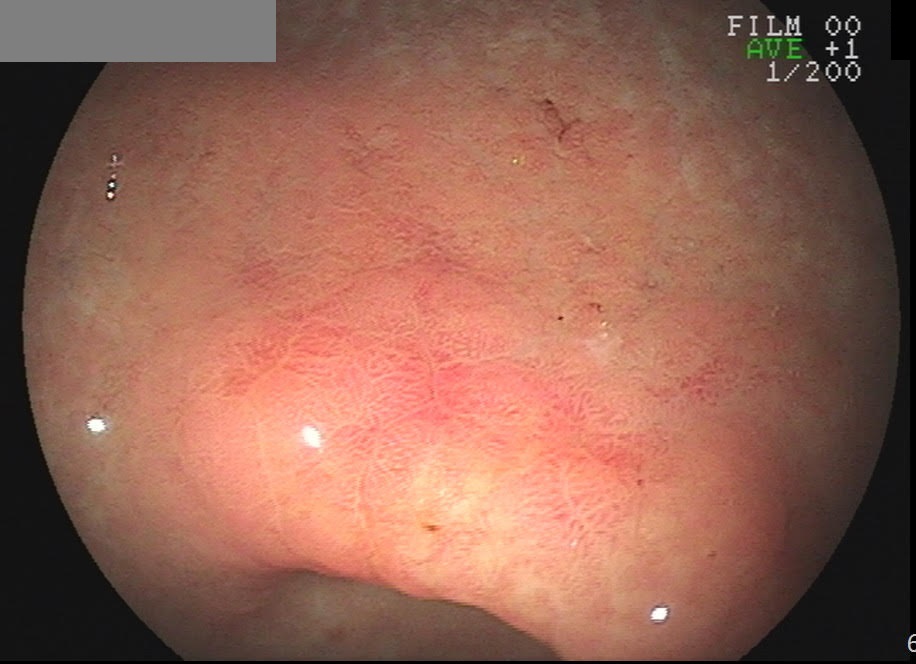
MALToma는 abnormal vessel이 특징입니다. Magnifying endoscopy로 관찰할 수 있습니다.
Staging workup을 어디까지 할 것인가에 대한 통일된 가이드라인이 없습니다. EUS로 T1/T2 나누어도 치료가 달라지지
Bone marrow involvement는 주로 multi-organ involvement가 있는 환자에서 발견됩니다.
[2020-10-21. 수다형 on-line talk show에서 나온 질문들]
[2021-5-4] MALToma 치료 후 헬리코박터에 대한 여러 질문
[2025-2-25] MALToma case review Maltoma에서 PET CT는 꼭 필요하다고 보시는지요?
[2025-2-25. 이준행 답변]
제 의견은 No입니다. Diffuse large B cell lymphoma에서는 PET 검사를 자주 시행하고 있습니다. 그러나 gastric MALToma에서 PET을 시행하지 않습니다. (1) 필요하지 않습니다. CT로 평가하면 충분합니다. (2) 심평의학에서 PET/CT 검사 시행을 허용하고 있는지 모르겠습니다. 과거에는 CT에서 뭔가 이상 소견이 있으면 추가로 PET/CT를 할 수 있는 것으로 되어 있었습니다. 자꾸 바뀌는 것 같고, 어짜피 필요하지 않아서 현재는 어떻게 되고 있는지 잘 모르겠습니다. 죄송합니다. (3) NCCN 2025년 가이드라인을 다시 찾아보았습니다. CT or PET/CT로 되어 있었습니다. CT를 하면 PET/CT를 할 이유가 없다고 생각됩니다. 요컨데 routine하게 검사하는 것은 권하지 않고 CT 유소견이나 기타 다른 이유가 있을 때에 한하여 selective하게 PET/CT를 하고 있습니다. (사실 거의 하지 않음)
2) Seifert E. Endoscopic and
bioptic diagnosis of malignant non-Hodgkin's lymphoma of the stomach. Endoscopy
1993
3) 정진태. 위 점막연관림프조직 림프종: 국내 치료 성적을 중심으로. 대한소화기학회지 2016
4) EndoTODAY Quiz on MALToma (2015-1-11)
5) EndoTODAY 위암 278 (2015-7-24)
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng
 [2017-1-24. 서울대 특강 질문]
[2017-1-24. 서울대 특강 질문]
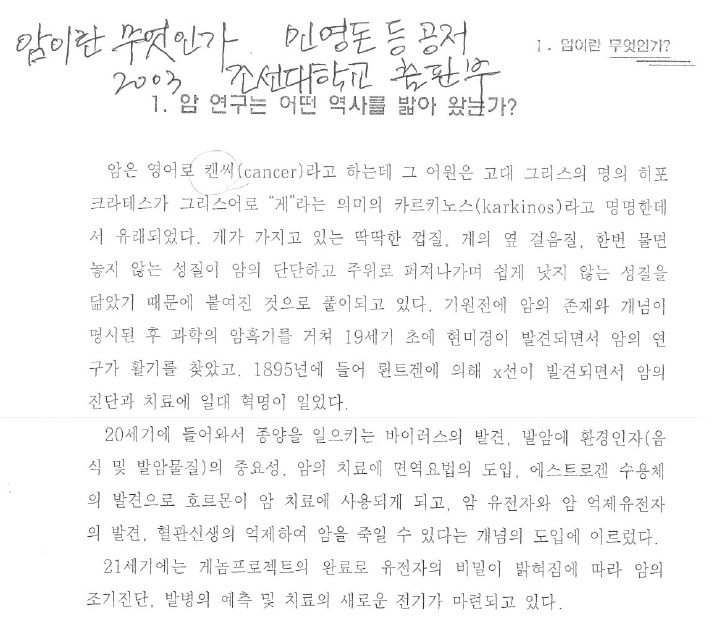 암을 왜 cancer라고 부르는지 그 기원을 잘 설명하고 있는 단행본
암을 왜 cancer라고 부르는지 그 기원을 잘 설명하고 있는 단행본
 [2017-1-24. 서울대 특강 질문]
[2017-1-24. 서울대 특강 질문]
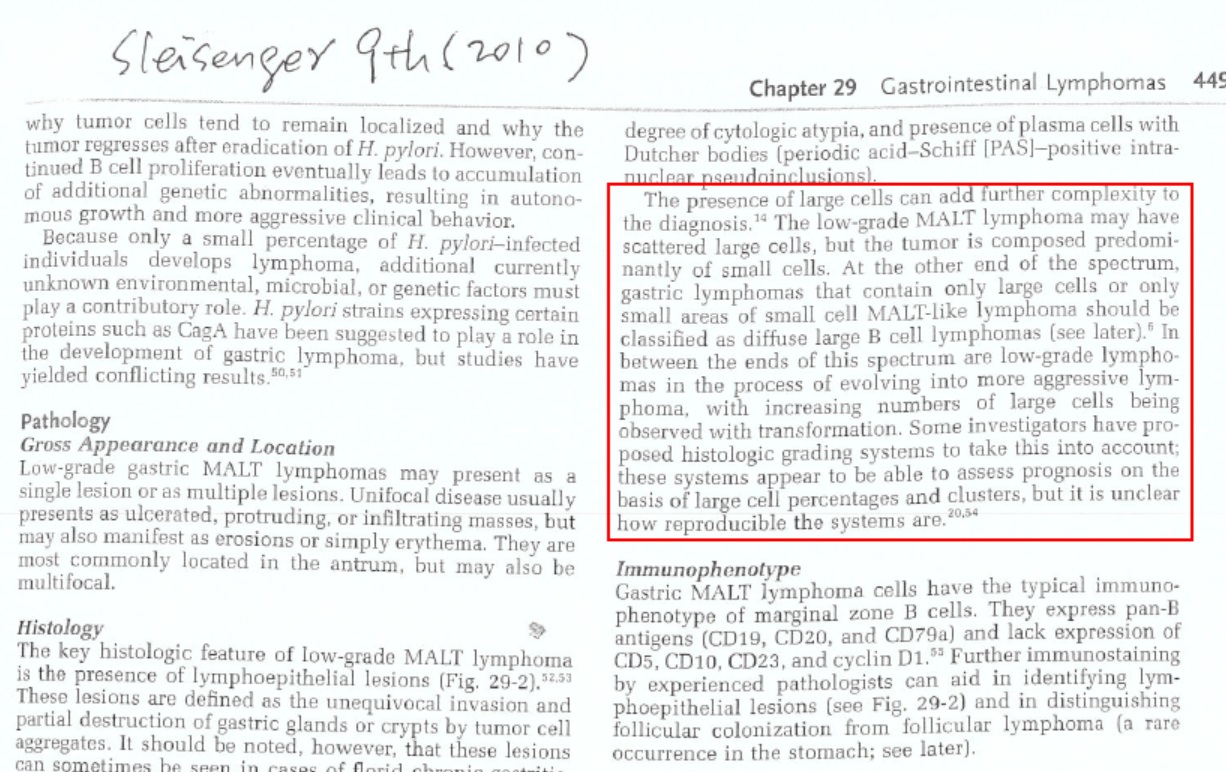 Sleisenger 9th (2010). MALT 림프종에 large cell component가 섞여 있는 경우에 대하여 비교적 상세히 논의되고 있음. MALToma와 diffuse large B cell lymphoma를 spectrum으로 설명하고 있음.
Sleisenger 9th (2010). MALT 림프종에 large cell component가 섞여 있는 경우에 대하여 비교적 상세히 논의되고 있음. MALToma와 diffuse large B cell lymphoma를 spectrum으로 설명하고 있음.
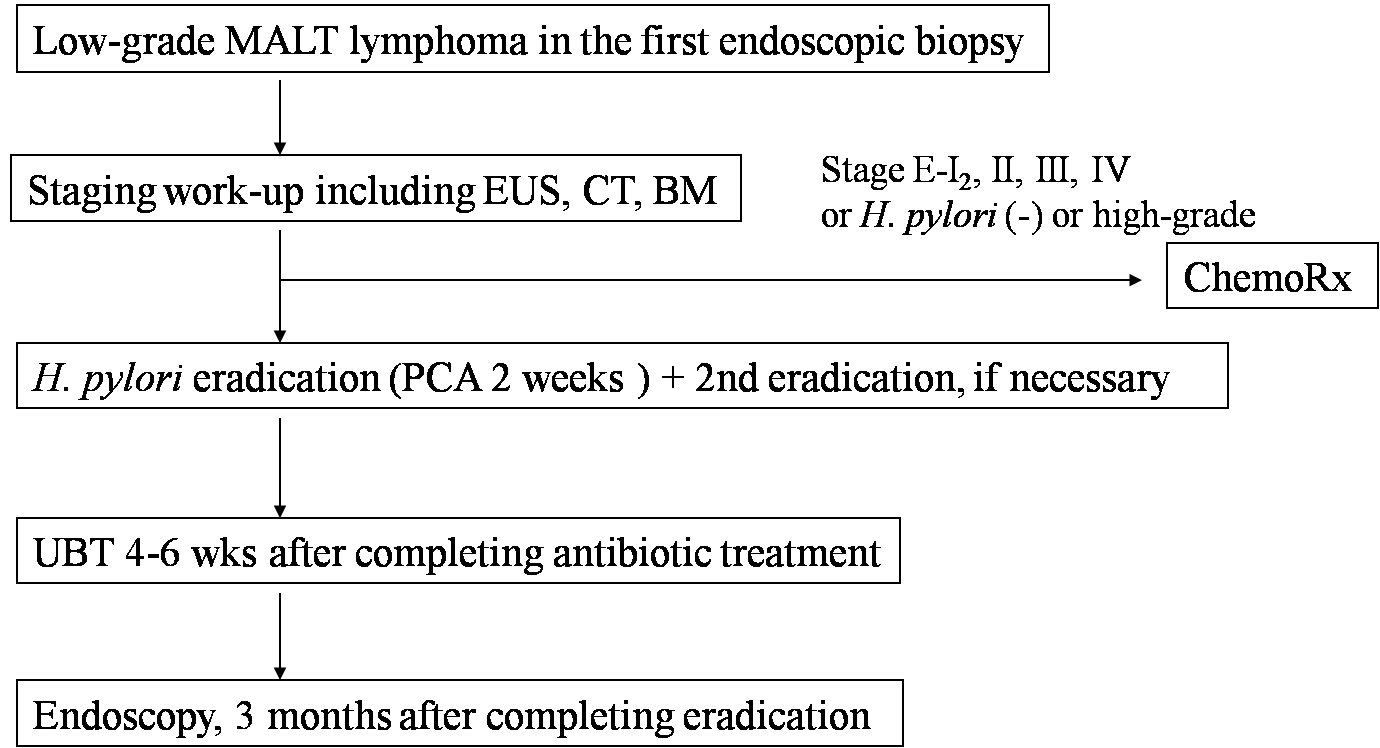 2005년 이전의 초창기 protocol. Proper muscle 이상을 침윤한 경우에는 항암치료를 선택하는 방식
2005년 이전의 초창기 protocol. Proper muscle 이상을 침윤한 경우에는 항암치료를 선택하는 방식
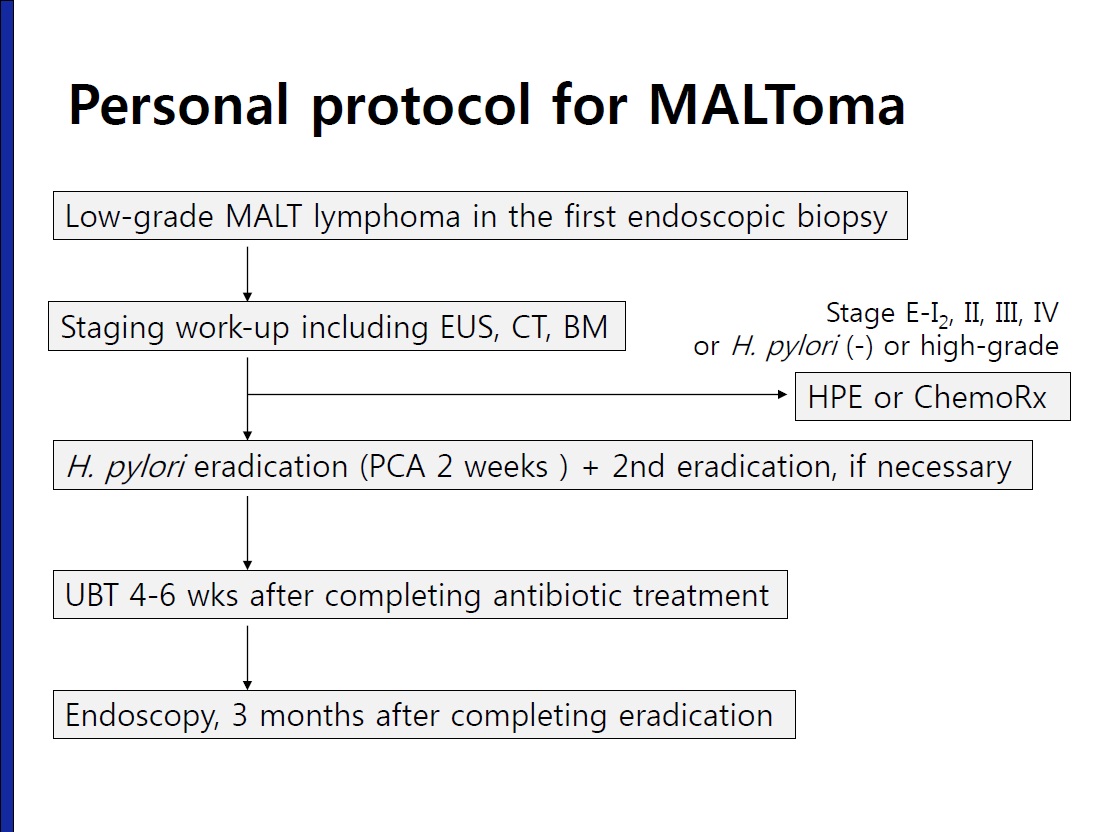 최근 사용하고 있는 protocol. Stage IE2 (proper muscle 이상의 침윤)에서도 대부분 일단 H. pylori 제균치료부터 시행하는 방식
최근 사용하고 있는 protocol. Stage IE2 (proper muscle 이상의 침윤)에서도 대부분 일단 H. pylori 제균치료부터 시행하는 방식
 Zucca. Ann Oncol 2013 - free PDF
Zucca. Ann Oncol 2013 - free PDF
2) 제균치료 성공률이 80% 전후인데 안 없어진 것으로 나오면 환자들이 급격히 irritable 해져서 잘 설명하고 치료하기가 어렵습니다. "암인데 그럼 죽으란 말이냐?" 질문하는 사람도 있습니다.
3) 1년이나 2년 기다려야 하는 사람도 있습니다. 개업가에서 어렵습니다.
4) 가끔 CT 찍어야 됩니다. 이 또한 어렵습니다.
5) 애매한 경우가 많습니다. 암이면 Lotto 복권인 사람도 있는데 애매한 경우는 대처하기 어렵습니다.
 에 대한 애독자 질문
에 대한 애독자 질문