 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [구강과 인후부. Oral cavity and laryngopharyngeal lesions] - 終
[구강과 인후부. Oral cavity and laryngopharyngeal lesions] - 終
1. 구강과 인후두 해부학
4. Laryngeal cancer - Total laryngectomy 후 내시경 소견
6. 이비인후과에서 hypopharyngeal cancer의 조직검사를 위하여 내시경 검사가 의뢰된 경우
7. Cases
8. FAQs
9. References
이비인후과에서 보는 것과 상하가 반대라고 생각하면 됩니다. 내시경으로 바라보면 vocal cord가 만드는 삼각형이 서 있습니다. 내시경을 보면 좌측이 좌측이고 우측이 우측입니다. 즉 좌우가 바뀌지 않습니다.
가장 자세한 설명입니다. World J Gastroenterol 2015
내시경 시야에 맞게 일부러 그림을 돌렸습니다. 내시경으로는 corniculate, cuneiform cartilage에 의한 돌출부가 보이지만 그 아래에는 arytenoid cartilage가 있어 vocal cord와 연결됩니다.
내시경학회 홈페이지에서 김도훈 교수님 강의 VOD 화면을 허락 없이 screenshot 하였습니다. 너무 좋아서... Sorry
간혹 아래와 같은 결과지를 봅니다. 인후부, vocal cord를 보지 못하였다는 comment입니다. 저는 이러한 comment는 필요하지 않다고 생각합니다. 현재 우리나라에서 인후부, vocal cord는 상부위장관 내시경 검사의 필수 관찰 영역은 아닙니다. 우연히 이 부위의 병소를 발견하면 사진과 기록을 남기겠지만, 이 부위를 보지 못했다고 또 다시 검사를 하거나 보지 못했다는 사실을 결과지에 남길 필요는 없다고 생각합니다. 상부식도부터 십이지장 (가능하면 제2부, 어려우면 제1부까지) 관찰하는 것이 무증상 성인 상부위장관 내시경의 검사 범위입니다. 인후부 증상이 있으면 인후부를 잘 봐주고 상복부 증상이 있으면 십이지장 제2부까지 꼭 보도록 권할 뿐이지 일반적인 screening endoscopy에는 적용되지 않습니다.
Uvula injury during EMR-C (2005)
Soft palate burn. 어제 뜨거운 차 마이면서 데었다.

Greater cornu of the hyoid bone (애독자 증례 편지 43)
Reinke's edema of the vocal cord is the swelling of the vocal cords due to fluid (edema) collected within the Reinke's space.
F/56. Tracheal stent seen in the GI endoscopy (2017)
목이 쉬었다는 증상을 가진 흡연력 많은 할머니의 검진이었습니다. 폐결절과 함께 supraglottic tumor를 발견하여 3차 병윈으로 전원한 사례가 있었습니다. (애독자 증례 편지 24)
아주대 이기명 교수님 팀에서는 epiglottis의 낭종에서 출혈하는 환자를 EVL로 지혈한 경험을 AJG에 보고하였습니다. 정말 훌륭한 시술입니다. A 51-year-old man was referred to our center following 5 days of fresh-blood hematemesis. Although esophagogastroduodenoscopy at admission failed to identify a lesion showing active bleeding up to the duodenum, hematemesis with hypovolemic shock occurred 10 hours later. An immediate laryngoscopic examination did not detect evidence of acute bleeding in the oropharyngeal space. A few minutes afterward, however, fresh blood flooded from the oral cavity. Endoscopic examination revealed active bleeding from the ventral surface of the epiglottis (a). An endoscope with a soft cap at its tip was carefully inserted into the epiglottic vallecula; examination showed a ~5-mm reddish, actively bleeding cystic mass in the deepest area of the left side of the epiglottic valeculla (b). While preparing the patient for immediate surgery, we attempted to arrest the hemorrhage endoscopically. An endoscope (GIF-XQ260, Olympus Medical, Tokyo, Japan), equipped with a band-ligating device, was carefully inserted into the bleeding site to avoid triggering the gag reflex. After cleansing the lesion by flushing with water, we tested whether suctioning the soft tissue around the lesion was sufficient for band ligation (c). Band ligation was performed while the lesion was suctioned into a device (d). The patient did not experience further bleeding. Follow-up endoscopic examinations after 2 days (e) and 2 weeks (f) showed band-ligated necrotic tissue and a flat whitish scar at the procedure site without any stigmata. To our knowledge, this is the first report of an epiglottic vallecular cyst presenting as acute bleeding and resolved via endoscopic band ligation. (Am J Gastroenterol 2017;112:414)
[Total laryngectomy 후 내시경 소견]
Total laryngectomy를 하면 oropharaynx와 식도가 direct하게 하나의 관처럼 연결됩니다.
출처: larykins.com.au
Adenoid cystic carcinoma로 total laryngectomy를 받은 분입니다. Oropharynx의 내시경 anatomy가 약간 변형되었지만 lumen을 찾아서 조심스럽게 들어가면 갑자기 식도가 나옵니다.
성대가 없으므로 인공 성대를 만드는 경우가 있습니다. 여러 방법이 있지만 Provox가 많이 사용되고 있습니다.
Provox를 사용하는 환자의 내시경 소견입니다.
| 2024-9-2. 하인두암 내시경 조직검사에 대한 의견 |
|
이비인후과에서 hypopharyngeal cancer 의심상태로 조직검사를 위하여 의뢰된 환자에서 EGD를 하면서 조직검사를 하는 일은 적지 않습니다. 위내시경 조직검사는 전신마취를 피할 수 있다는 점에서 환자에게는 상당히 유리한 조직검사 방법입니다. 그러나 건진 내시경에서 우연히 hypopharyngeal cancer 의심병소가 발견되면 그 자리에서 즉시 조직검사를 하는 것은 무척 어려운 일입니다. 위내시경은 인후두암 검사는 아니기 때문이고 해당 설명이나 동의서도 없기 때문입니다. 대부분 고령이고 뭔가의 underlying disease가 있는 환자가 많다는 점도 고려해야 합니다. 내시경 의사가 정말로 자신이 있으면 조직검사를 해도 좋습니다. 그러나 조금이라도 우려점이 있으면 이비인후과로 의뢰하는 것도 나쁘지 않은 선택입니다. 비록 이비인후과에서 전신마취하 LMS biopsy에 앞서 EGD biopsy를 권유하여 다시 내시경실로 오는 한이 있더라도... |
(2015) Screening endoscopy에서 발견된 hypopharyngeal cancer
(2019) 여자 72세. Screening endoscopy에서 발견된 hypopharyngeal cancer (left pyriform sinus squamous cell carcinoma)
상기 환자 이비인후과에서 LMS 하 조직검사 시행
11년 전 식도암 수술받은 환자의 hypopharynageal cancer. 5일 전부터 여러번 다량의 토혈을 했다고 함.
Squamous cell carcinoma. T2N1, Stage III. 3년 후 흉통이 발생하였고 식도암이 확인되었습니다.
CCRT 후 CR이 왔으나 stricture로 고생하고 dilatation 등 치료를 하다가 결국 수술을 받은 환자입니다 (2015).
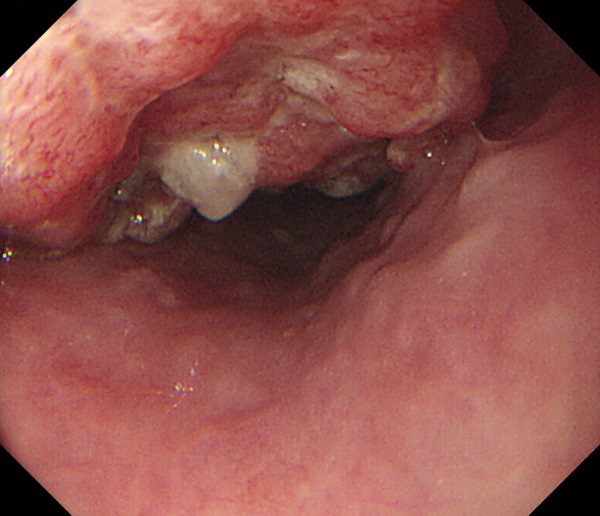
(2015) 30PY 흡연력을 가진 남성으로 반년 전부터 우측 목의 통증이 있어 인근 이비인후과를 방문하여 치료받았으나 호전이 없었고 목소리도 쉬기 시작하여 본 병원 이비인후과를 방문하셨습니다. 이비인후과 진찰 후 right pyriform sinus 암 의심으로 조직검사와 식도부위의 synchronous cancer 여부를 확인하기 위하여 상부위장관 내시경 검사가 의뢰되었습니다. 이비인후과에서 찍은 사진은 좌우가 바뀌기 때문에 내시경 의사로서는 방향잡기가 어렵습니다. 이비인후과의 사진을 180도 돌리면 좌우가 바뀌지 않은 사진, 즉 내시경을 삽입할 때와 같은 편안한 방향이 나오므로 쉽게 orientation을 잡을 수 있습니다.
Flexible upper GI endoscope로 더 자세히 관찰할 수 있었으며 조직검사에서는 moderately differentiated squamous cell carcinoma로 나왔고 식도에서는 또 다른 병소는 없었습니다. CCRT 시행하였습니다. Hypopharyngx의 병소는 이비인후과에서 조직검사가 어렵기 때문에 (이비인후과에서는 조직검사를 위하여 전신마취를 해야 한다고 합니다), 조직검사를 하고 식도도 살필 겸 위장관내시경이 의뢰되고 있습니다. 조심스럽게 target biopsy를 하면 진단을 붙일 수 있습니다. 이 환자의 laryngoscopy 사진은 아래와 같습니다. 내과에서 위내시경으로 찍은 사진과 이비인후과에서 laryngoscopy로 찍은 사진의 좌우가 반대라는 것을 알 수 있습니다. 위내시경에서는 좌우가 바뀌지 않습니다.
(2015) 우측 pyriform sinus cancer 환자에서 발견된 superficial esophageal cancer
[최근 내시경에서 발견하지 못하였던 hypopharyngeal cancer]
[게실]
만성적으로 식후 오른쪽 목에 이물감을 느꼈고 손으로 조작하면 빠지는 느낌이었다는 60대 여성입니다. 내시경에서 fistula 의심되었지만 esophagography에서는 left pyriform sinus diverticulum이었음.
[이물에 의한 상부식도 천공]
15년 전 경추 수술 (anterior fusion, C4-5-6) 후 연하 장애가 있는 분의 내시경에서 upper esophageal sphincter 직하방에서 metalic foreign body가 발견되었음. 식도 후벽 천공으로 진단하고 NS에서 metaplic plate와 screw를 제거한 후 이비인후과에서 supraclavicular muscle flap을 이용하여 perforation repair 시행함
 6. 이비인후과에서 hypopharyngeal cancer의 조직검사를 위하여 내시경 검사가 의뢰된 경우
6. 이비인후과에서 hypopharyngeal cancer의 조직검사를 위하여 내시경 검사가 의뢰된 경우
이비인후과에서 hypopharyngeal cancer의 조직검사를 위하여 내시경 검사가 의뢰되는 경우가 있습니다. Hypopharyngeal area는 이비인후과에서 관찰은 쉽게 할 수 있지만 조직검사를 위해서는 전신마취가 필요한 환자가 많다고 합니다. 내시경 시행 의사의 입장에서 내시경을 안정적으로 위치시키기도 어렵고 혹시 출혈을 하면 지혈이 어렵기 때문에 마음의 부담이 클 수 밖에 없습니다. 걱정이 됩니다. 그러나 대부분의 경우 출혈이 많지 않고, 혹시 출혈되더라도 aspiration만 심하지 않으면 이비인후과로 의뢰하면 그쪽에서 적절히 조처할 수 있습니다. 따라서 이비인후과에서 의뢰된 환자는 돌려보내지 말고 가급적 조직검사를 해 드리는 것이 좋겠습니다.
Left pyriform sinus 영역의 NK-T cell lymphoma 재발로 조직검사를 위하여 내시경 검사가 처방된 경우입니다. 상부 내시경 조직검사로 진단되었고 치료가 시작되었습니다.
이비인후과 사진은 좌우가 바뀌는 반면, 위내시경은 좌우가 바뀌지 않는다는 점을 잊지 않으면 되겠습니다.
[2017-8-25. 추가] 이 검사를 했던 fellow 선생님과 이야기를 나누었는데... 아래와 같은 메일을 주셨습니다.
네 교수님 이환자분이 기억이 납니다. 저도 이비인후과에서 조직검사를 의뢰 받은게 처음이라... 다행히 병변은 위내시경으로 확인이 잘되는 위치에 있었고 조심스레 tissue를 뜯었을때 bleeding도 많지 않았었습니다. 조직검사 후에도 흡인에 대한 염려때문에 잠깐이라도 내시경으로 살펴보았고, 환자를 앉혀서 내보냈었습니다. 조직검사로 병이 잘 확인되어서 참 다행입니다.
[Case] Right pyriform sinus cancer (EsoTODAY 023)
위내시경은 주로 left pyriform sinus를 통하여 식도로 들어갑니다. 따라서 간혹 left pyriform sinus cancer를 발견하는 경우가 있습니다. 반면 right pyriform sinus cancer를 내시경으로 발견하는 것은 드문 일입니다. 특별히 주의하여 관찰하지 않으면...
검진 내시경에서 우연히 right pyriform sinus cancer가 의심되어 이비인후과로 의뢰되었던 환자입니다.
이비인후과에서 저희 소화기내과로 조직검사를 위하여 의뢰가 되었습니다.
내시경 재검을 하였고 병소가 명확히 관찰되어 조직검사를 하였습니다. 약간의 출혈은 있었으나 곧 멈추었습니다.
하인두의 일부인 pyriform sinus 병소 조직검사를 이비인후과에서 소화기내과로 의뢰한 것에 대하여 의아해 하실 분이 계실 것 같습니다. 그러나 간혹 있는 일입니다. 이 부위 병소의 조직검사는 이비인후과에서도 어려워합니다. 이비인후과에서도 전신마취를 한 상태에서 조직검사를 하고 있습니다. 그래서 소화기내시경실로 의뢰가 오는 것입니다. 약간 겁나지만... 충분히 할 수 있는 일입니다. Sedation을 깊게 하지 않으면 약간 출혈이 되더라도 문제가 없습니다.
[Case] Tuberculous (TB) pharyngitis with lymphadenitis (EsoTODAY 022)
40대 남성입니다. 목이 불편하고, 덩어리지고 큰 것을 먹을 때 아프다는 증상으로 이비인후과 fellow 선생님 외래를 방문 후 조직검사가 시행되었고 다음의 소견이었습니다. "Pyriform sinus, left, punch biopsy: Chronic inflammation and inflamed granulation tissue."
이비인후과에서 시행한 CT에서는 다음과 같이 판독되었습니다.
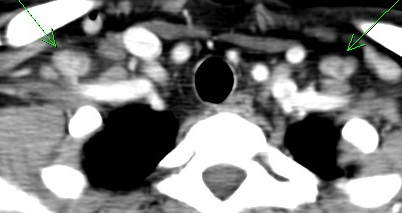
소견: Left pyriform sinus에 2.7 cm 가량의 heterogeneously enhancing soft-tissue mass가 관찰되며 이 mass는 pyriform sinus의 apex까지 extension 되어 있음. Left neck의 IIa와 양측에 supraclavicular fossa에 multiple variable sized heterogeneously enhancing lymphadenopathy가 관찰됨.
Impression: Left pyriform sinus cancer with bilateral multiple lymph node metastases (T2 N2c)
식도 질환 유무를 확인하기 위하여 내시경 검사가 의뢰되었습니다. 식도는 정상이었고 post-cricoid area부터 left pyriform sinus media wall에 걸쳐 white plaque를 보이는 하인두 점막 염증 소견이 관찰되었습니다.
"Left pyriform sinus에 buling 및 whitish patch lesion 있어 fiberoptic guided biopsy 하였습니다. biopsy 상에서는 Chronic inflammation 소견 pending EBV 소견이나 ROF CT 상 Left pyriform sinus cancer with bilateral multiple lymph node metastases (T2N2c)" 소견으로 종양 전문 이비인후과 교수님께 의뢰된 후 수술(diagnostic laryngomicroscopic surgery with biopsy + excisional biopsy of cervical lymph node)이 시행되었습니다.
최종 병리결과는 "(1) Left pyriform sinus: Chronic inflammation, Multiple granulomas and multiple granulomatous vasculitis, (2) Lymph nodes, level III: Two reactive lymph nodes"로 나왔는데 함께 의뢰된 Tuberculosis PCR 검사에서 양성으로 나와 TB pharyngitis with lymphadenitis로 진단할 수 있었습니다. 항결핵치료 후 호전되었습니다. 추적 위내시경은 받지 않으셨고 이비인후과에서 laryngoscopy 검사 사진을 남기셨습니다.
사족일지 모르지만, 이 증례를 laryngeal tuberculosis로 불러야 할지 pharyngeal tuberculosis로 불러야 할지 살짝 고민이 되었습니다. 크게 달라질 것은 없겠지만 위내시경 의사의 입장에서 보면 주된 위치가 hypopharynx로 생각되었기 때문입니다. 그래서 다들 laryngeal TB로 불렀지만 저는 진단명을 pharyngeal TB로 생각하고 있습니다.
[Case] Diffuse idiopathic skeletal hyperostosis
73 years old male complained chronic swallowing difficult. In the endoscopy, no specific mucosal lesion was found. In the spine CT, severe degenerative change with prominent anterior bridging spur compressing the pharynx was found. After surgical decompression, the symptom was relieved.
[2017-4-1. 애독자 질문]
식도 게실을 유심히 관찰하여 보고한 fellow 선생님을 소개해 주셨는데요 (EsoTODAY 020), 오늘 저희 병원 fellow 선생님도 검진 내시경을 회수하던 중 우측 이상동에서 종괴를 발견하여 제게 보고하였습니다. 저는 내시경을 삽입하다 생긴 혈종 같다고 말했는데, 본인은 우측으로 넣은 적이 없다고 하여 다시 자세히 보니 혈종이 아니고 보라색의 종괴였습니다. 검사를 바쁘게 하다 보면 내시경 회수를 서두르다 후두 관찰을 제대로 못하는 경우가 있는데, fellow 선생님께서 용케 잘 찾아낸 것 같습니다.
구글 검색을 해보니, laryngeal hemangioma 사진(Wang Oncol Lett 2011 Figure 1)이 이와 유사한데, 본 환자도 hemangioma 일지요? 이 교수님 고견을 구합니다.
조직검사를 시행해도 될지요? 왠지 피가 많이 날 것 같은 걱정이 듭니다만, 생검을 하지 않으면 진단하기 어려울 것 같습니다. 상기 증례보고에서는 ENT에서 resection 후 병리 진단으로 확인하였습니다. 더 건드리지 않고 ENT로 보내는 것이 현명할지요?
[2017-4-2. 이준행 답변]
저도 hemangioma라고 생각합니다. 그런데 꼭 조직검사가 필요하지 모르겠습니다. 이비인후과에 의뢰하여 경과관찰 하는 방향이 어떨까 싶습니다. 원하시면 소화기내과에서 경과관찰 할 수도 있지만... 아무래도 전문 진료과에 의뢰하는 것이 제 스타일입니다. 볼 수 있다고 다 우리 영역은 아니니까요. 피부는 내과 의사도 볼 수 있지만 피부병을 내과에서 주로 진료하지 않는 것과 같다고 할 수 있습니다.
이 부위의 병소는 이비인후과에서도 조직검사를 어려워합니다. 전신마취하 조직검사를 하는 것 같습니다. 간혹 이 부위에 암이 발견되면 오히려 이비인후과에서 소화기내과로 의뢰를 하기도 합니다. 소화기 내시경으로 조직검사를 하기가 더 쉽기 때문입니다. 그렇지만 hemangioma가 의심되는 상황이므로 건드리지 않는 것이 상책이라고 생각됩니다. 감사합니다.
[2016-6-12. 애독자 편지]
이번 인후부 병변에 대해서 보내주신 것을 보고 저도 증례 하나 보내드립니다. 60대 남성분 검진으로 한 위내시경에서 right hypopharynx에 mass 관찰되어 바로 대학병원 ENT로 진료의뢰하여 가신 분입니다. 구강암이라는 이야기 들었다는 소식까지 들었습니다.
사실 1년 전 저희 병원에서 위내시경을 받으셨는데 그 때 인후부 찍은 사진이 없었습니다. 그 당시부터 병변이 있었는지 없었는지는 모르지만 한참을 마음이 불편했습니다. 구역질이 심하시거나 협조가 어려우면 인후부는 찍지 않고 그냥 식도로 넘어간 적도 많은데 이 이후로는 모든 환자의 인후부를 잘 보려고 노력하고 있습니다.
[2016-6-13. 이준행 답변]
좋은 증례 감사합니다. 정말 마음 착한 선생님 같습니다. Blind 하게 삽입하였더라면 이번에도 놓치기 쉬운 병소를 잘 찾으셨습니다. 1년 전 사진이 없는 것을 보고 마음이 아프셨다니... 그 착한 마음 늘 간직하시기 바랍니다.
사실 인후부는 들어갈 때나 나올 때 모두 자세히 관찰하기 어렵습니다. 특히 conscious sedation 보다 깊은 정도로 sedation된 환자에서는 더욱 어려운 것 같습니다. 그래서 저도 인후부를 자세히 관찰하지 못하고 있습니다. 노력은 합니다만 잘 되지 않는다는 이야기입니다.
내시경으로 인후부 병소를 발견하면 잘 한 일이지만, 내시경으로 인후부 병소를 발견하지 못했다고 자책하실 이유는 없습니다. 상부 내시경의 주된 검사 범위는 위, 식도, 십이지장이니까요.
뻔한 병소는 놓치면 문제고 발견하면 당연한 일입니다. 어려운 병소는 놓칠 수 있습니다. 발견한 사람이 대단한 것이지요. 인후부 병소는 후자입니다.
[2018-12-30. 애독자 편지]
최근 조기위암 내시경치료 후 follow-up 중인 환자에서 인후부암을 발견하였습니다. 검사 당시에는 benign에 가깝다는 생각을 지울 수 없었습니다. Squamous epithelium 부분이라 adenoma가 생기는 곳은 아니었지만, 아주 드문 membranous basal cell adenoma arose from the minor salivary glands in the oro- or hypopharynx를 생각하다보니 adenoma라고 붙였던 것 같습니다. 그리고 oro-pharynx와 hypopharynx의 경계가 궁금합니다.
[2018-12-30. 이준행 답변]
위 질환 환자에서 무증상 인후부 질병을 발견하신 것만으로도 아주 훌륭한 일을 하셨습니다. 말씀주신 바와 같이 adenoma가 생기는 부위는 아니므로 impression이 조금 이상하기는 합니다. 여하튼 잘 하셨습니다.
사실 이 환자의 병소는 pharynx가 아니라 larynxr가 아닌가 생각합니다. 음식 넘어가는 곳이 pharynx, 공기 통로가 larynx라고 한다면 아무래도 larynx에 가깝지 않을까요?
Pharynx 중 epiglottis top 보다 아래를 hypopharynx라 부릅니다.
[2021-7-20. 이준행] 인후부 이물감은 대부분 과민성입니다.
2) 홍현준 (이비인후과). 내시경 의사를 위한 구강 및 인후두의 해부와 생리 (내시경세미나)
3) 성대의 접촉성 육아종 환자에서 칼륨 경쟁적 위산 분비 차단제의 처방 강동 경희대병원 이영찬. PDF
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.