 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [색소내시경. Chromoendoscopy] - 終
[색소내시경. Chromoendoscopy] - 終
1. Introduction
2. How to apply the dye onto the lesion
3. Premedication with pronase in EGD
★ 4. Lugol solution - Esophageal mucosal cancer, Esophageal submucosal cancer, Advanced esophageal cancer, Pink color sign, Barrett's esophagus, Side effects
5. Indigo carmine - Gastric adenoma and cancer, Bleeding by spraying, Is rountine spraying of indigo carmine helpful?
6. Acetic acid for GI chromoendoscopy
8. FAQ
9. References
색소내시경은 작용기전에 따라 아래와 같이 3 가지로 나누어집니다. Tattooing agents를 포함하여 4 가지로 나누기도 합니다.
색소내시경은 아니지만 melanosis coli 환자에서 작은 선종이 쉽게 발견되기도 합니다. 천연색소라고 할 수 있겠지요.
 2. How to apply the dye onto the lesion
2. How to apply the dye onto the lesion
1) Biopsy channel로 주입
색소를 뿌리는 가장 쉬운 방법은 syringe에 색소를 넣은 후 biopsy channel로 주입하는 것입니다. Biopsy channel을 volume 때문에 10ml를 넣으면 조금밖에 뿌려지지 않습니다. 이 때 공기를 10ml 쏴주면 lumen 내의 dye가 뿌려집니다. 저는 gastric ESD할 때 늘 이 방법을 사용합니다.
2) Spayer
색소는 보통 sprayer를 써서 뿌립니다. 간혹 너무 강하게 뿌리면 출혈이 발생할 수 있습니다. 시간이 많이 걸리고 sprayer 사용에 따른 추가 비용도 있습니다.
3) Injector needle
저는 종종 injector needle을 사용합니다. 물이 흐르는 방향을 잘 고려하여 needle을 병소 옆에 가져댄 후 천천히 dye를 흘리는 것입니다. 여러분도 시도해 보십시오.
 3. Premedication with pronase in EGD
3. Premedication with pronase in EGD
위에 점액이 붙어있으면 상세한 관찰과 정확한 조직검사가 어렵습니다. 주사기로 물을 뿌려보지만 만족스럽지 못한 경우가 많습니다. 내시경 검사 전 proteinase가 포함된 액체를 마시면 위의 점액이 감소되어 위벽을 깨끗하게 관찰할 수 있습니다.
일본에서는 거의 항상 이용되고 있는 모양인데 국내에서는 사용 빈도가 낮습니다. 이유는 많겠지만, 우리나라의 유일한 내시경 용 pronase (상품명 Endonase F)가 아직 보험 급여가 아닌 것이 중요한 문제일 것 같습니다.
건국대학교 이선영 교수님과 순천향대학교 정일권 선생님께서 Endoscopy지의 흥미로운 논문을 소개합니다. 제목은 Endoscopic flushing with pronase improves the quantity and quality of gastric biopsy: a prospective study입니다. 조직검사 전 pronase로 flushing하면 조직검사의 질이 좋아진다는 내용이었습니다. 요약을 옮깁니다.
Background and study aims: Pronase, a proteolytic enzyme, is known to improve mucosal visibility during esophagogastroduodenoscopy (EGD), but little is known about its effects on gastric biopsy. This study assessed whether endoscopic flushing with pronase improves the quality of gastric biopsy. Patients and methods: Consecutive patients who underwent EGD were randomly assigned to either the control group or the pronase group in a prospective setting. The first biopsy of the identified lesion was performed during endoscopy. Endoscopic flushing with either 50mL of water and dimethylpolysiloxane (DMPS; control group) or 50 mL of water, pronase, sodium bicarbonate, and DMPS (pronase group) was then applied to the lesion. After 5 minutes, the second biopsy was performed 2-3 mm away from the first biopsy site. The thickness of mucus, depth of the specimen, overall diagnostic adequacy, anatomical orientation, and crush artifact were measured to assess the quality of the biopsy. Results: Of the 208 patients, 10 were not analyzed due to the absence of an identifiable lesion. Compared with the control group, the pronase group showed significantly decreased thickness of mucus (P<0.001), increased depth of biopsy (P<0.001), improved anatomical orientation (P=0.010), and improved overall diagnostic assessment (P=0.011) in the second biopsied specimen following endoscopic flushing. The crush artifact and hemorrhage did not differ between the groups. Conclusions: Endoscopic flushing with pronase not only improved the depth of biopsy but also the anatomical orientation and overall diagnostic adequacy. Pronase can be recommended for flushing during EGD to improve the quantity and quality of biopsy.
우리나라에서는 아직도 (2019년 8월 현재) pronase (Endonase F)가 비보험(인정 비급여 - 2,300원 정도)인 것이 문제입니다. 고가인 Endonase F가 아닌 일반 거담제라도 사용하면 좋겠지만 규정 상 이마저 쉽지 않습니다. 적응증에 포함되어 있지 않으므로....... 결국 Endonase F의 가격을 낮추고 보험급여로 전환하여 모든 내시경 검사에서 기본적으로 사용하는 방식이 좋지 않을까요?
어쩌면 알기론이나 가소콜보다 엔도나제가 더 중요할지 모른다는 생각이 듭니다. (2019-8-19. 이준행)
[2022-8-10] 삼성서울병원에 Endonase가 도입되었습니다. 아직은 비급여이므로 꼭 필요한 환자에서 선택적으로 사용해볼 생각입니다. 이렇게나 필수적인 약제가 아직도 비급여라는 사실에 좌절감을 느낌입니다.
 4-1. How to use Lugol chromoendoscopy
4-1. How to use Lugol chromoendoscopy
색소내시경 중에서 가장 유용한 것이 루골액과 인디고카민입니다. 루골액부터 시작하겠습니다.
루골액은 Jean Guillaume Auguste Lugol의 이름에서 기원되었습니다. 루골액의 iodine이 nonkeratinized squamous epithelium의 글리코겐에 affinity를 가지고 있기 때문에 식도내시경에서 사용되는 것입니다. 정상 식도상피는 갈색으로 염색되지만 이형성이나 암이 되면 루골액이 흡착되지 않습니다 (Lugol void area). 약한 이형성에서는 중간정도의 색깔을 보일 수 있습니다. 보통 2 - 3 % 용액을 5 - 10 mL 정도 사용합니다.
루골 색소내시경의 tip은 색소분무 후 공기를 흡인하여 내강을 collapse시키고 30초 정도 기다리는 것입니다. 루골액을 식도점막에 골고루 접촉시키기 위함입니다.
생리식염수로 흡착되지 않은 루골액을 씻어내라는 책도 있습니다. 그러나 생리식염수로 씻지 않아도 충분한 contrast가 나오는 것 같습니다. 생리식염수를 쓰면 오히려 contrast가 낮아질 수 있으므로 저는 거의 사용하지 않고 있습니다.
식도암 내시경치료 전 경계판정에 루골액은 필수입니다.
조건에 따라 약간 다른 느낌의 갈색으로 보입니다.
2.5 cm 식도암으로 SM invasion이 있었습니다.
[2017-4-12. 루골 사용 protocol 다시 확인 함]
 4-2. Esophageal mucosal cancer cases of Lugol chromoendoscopy
4-2. Esophageal mucosal cancer cases of Lugol chromoendoscopy
 4-3. Submucosal cancer cases of Lugol chromoendoscopy
4-3. Submucosal cancer cases of Lugol chromoendoscopy
 4-4. Advanced esophageal cancer cases of Lugol chromoendoscopy
4-4. Advanced esophageal cancer cases of Lugol chromoendoscopy
진행성 식도암에서는 조기식도암의 경우보다 루골액의 유용성이 낮지만 간혹 white light endoscopy에서 보이는 것보다 훨씬 넓은 병소가 확인되는 경우는 있습니다.
Proper muscle invasion (+)
Proper muscle invasion (+)
식도에 고루 Lugol을 분무하면 간혹 white light endoscopy에서 그다지 의심하지 못했던 표재성 식도암을 발견하기도 합니다.
상절치 33-36cm에 진행성 식도암이 있어 의뢰된 환자입니다. Lugol spray 후 28-30cm에서 표재성 식도암을 추가로 발견하였습니다. 조직검사는 모두 M/D squamous cell carcinoma였습니다.
 4-5. Pink color sign in Lugol chromoendoscopy?
4-5. Pink color sign in Lugol chromoendoscopy?
루골액에 염색되지 않은 부위를 수 분간 관찰하면 색조가 연해집니다. Pink 빛으로 연해지면 식도암이라는 설이 있습니다. Pink color sign이라고 합니다.
일본인들은 간혹 너무 주관적인 주장을 하기도 하는데 pink color sign도 그러한 경우 같습니다. 저는 큰 의미를 주지 않고 있습니다. 무시하기를 권합니다.
 4-6. Lugol chromoendoscopy for Barrett's esophagus
4-6. Lugol chromoendoscopy for Barrett's esophagus
루골액은 squamocolumnar junction의 contrast를 강조시킵니다. 과거에는 가끔 바렛식도를 관찰하는데 이용하였습니다.
루골액을 이용한 바렛식도 관찰
최근에는 바렛식도의 진단을 위하여 루골액을 사용하지 않고 있습니다. 이유는 두 가지입니다. (1) 일반 white light endoscopy도 바렛식도를 관찰하는데 충분합니다. (2) 강조영상을 얻고 싶다면 NBI를 이용할 수 있습니다. 훨씬 간단한데 루골액 못지 않게 좋은 영상을 얻을 수 있습니다.
NBI를 이용한 바렛식도 관찰
바렛식도에서 루골액을 쓰지 마십시요. 비용-효과를 고려하십시요. 같은 이유로 역류성 식도염이나 sentinel polyp을 잘 보기 위하여 루골액을 쓸 필요는 없다고 생각합니다.
[참고] NBI에 대한 YouTube 자료
 4-7. Side effects of Lugol chromoendoscopy
4-7. Side effects of Lugol chromoendoscopy
색소내시경에 부작용은 없는지 문의하신 분이 계십니다. 세상일에 100% 안전이란 없는 법이니 색소내시경도 분명 부작용이 있을 것입니다. 2010년 아산병원 증례를 소개합니다 (대한소화기내시경학회지 2010;41:224).
"루골 용액의 가능한 부작용으로는 오심, 구토, 심와부 및 상복부 통증 등이 있고 드물게 화학성 식도염이나 위염이 발생할 수 있다. 일반적으로 색소내시경시 0.5∼5%의 요오드가 포함된 루골 용액 10∼30 mL를 식도에 산포한다. Sreedharan 등은 3∼5%의 높은 요오드 농도의 용액에서 점막 손상이 잘 발생하므로, 1.5% 정도로 요오드가 낮은 농도의 용액을 10∼20 mL 사용함으로 점막 손상을 줄일 수 있다고 제안하였다. 그러나 급성 식도 또는 위 점막 손상이 1.0∼1.5%의 낮은 농도의 루골 용액을 사용한 증례에서도 보고되었다. 점막 손상은 1.0∼1.5%의 낮은 농도의 루골 용액을 사용한 경우에는 1∼2일 후 발견되었지만 5.0%의 높은 농도의 루골 용액을 사용한 증례에서는 검사 도중 루골 용액의 흡인을 위해 위 내로 재진입 하였을 때 점막의 손상이 확인되었다. 루골 용액으로 인한 점막 손상은 루골 용액 산포 시점과 위 재검 시점 사이의 시간 간격이 길어짐으로써 루골 용액의 위 잔류시간이 길어진 경우 쉽게 발생할 수 있지만, 본 증례와 Sreedharan 등의 보고와 같이 고농도의 용액을 사용한 경우에는 위 재검까지의 시간 간격이 짧더라도 점막 손상이 생길 수 있음을 알 수 있다."
색소내시경 후 부작용이 발생할 수 있지만 그 빈도는 낮습니다. 부작용 우려 때문에 검사를 피할 정도는 아니고 다만 너무 높지 않은 농도를 사용하고 남은 용액은 흡인하면 좋을 것이라 생각합니다.
4-8. Lugol solution 공급에 대하여 (2016-4-14)
과거에는 루골 용액을 각 병원에서 조제하여 사용하였습니다. 그러나 그 재료가 의료용으로 허가받은 것이 아니라는 지적이 있어서 상당기간 사용하지 못하고 있습니다. 그 대안으로 5% 루골액인 젬스테인 용액(1병당 10ml, 2만 7천원)을 고려할 수 있습니다. 적응증이 '갑상선 기능 항진증에 대한 수술 전처치'로 허가 받은 제품인지라 색소내시경 진단용으로 사용해도 적절한지는 잘 모르겠습니다. 아마 비급여로 써야 할지도 모릅니다. 조속히 적응증이 확대되어야 할 것 같습니다.
[루골 용액 시판약으로 사용하기로 함 (2016-7-11)]
안전성 문제로 루골 용액을 조제하여 사용하는 것이 금지되었습니다. 대안으로 시판약을 써야 하는데 급여 처방이 되지 않아서 환자 부담은 증가되었습니다. 생색은 정부에서 내고 바쁜 말은 병원에서 듣고 비용은 환자가 내는 어처구니 없는 정책이라고 생각됩니다.
소화기내과 선생님들께 (참조, 흉부외과 교수님들께),
내시경 검사 중 식도암 또는 식도암 의심병소가 있을 때 이제까지 원내 제조 1% Lugol solution을 무수가로 사용해 왔었으나 금일 부터는 안전성의 문제로 필요시 시판약을(한국콜마 젬스테인 용액) 비급여(24200원) 처방하여 사용해야 합니다.
내시경실에 비품을 두기 때문에 사용에는 문제가 없겠으나 처방시 환자 또는 보호자에게 의사가 직접 설명을 해드려야 합니다. 따라서 식도암으로 내시경을 시행하는 경우 검사 시작전에 미리 비급여 처방에 대해 알려드리는 것이 좋겠고 검사 중 예기치 않게 사용하게 될 경우 보호자(없다면 환자)에게 따로 비급여 처방으로 염색약 사용이 필요함을 설명드려주십시오.
젬스테인 용액(코드:LUGO5-S)은 병에 5% iodine 10ml가 들어 있습니다. 지금까지 Iodine을 1%로 희석하여 잘 사용해왔었으므로 앞으로도 5% iodine을 1:4로 희석(5배 묽게)해서 사용하면 되겠습니다.
Indigo carmine은 제가 가장 사랑하는 색소입니다. 거의 매일 사용하고 있습니다. 다음은 루골액입니다. 그러나 사용 빈도가 다릅니다. Indigo carmine이 없는 ESD는 생각만 해도 끔직합니다. 그런데 저는 아직 indigo carmine의 정확한 기원조차 모릅니다. 혹시 정확한 정보를 가지신 분은 제게 연락주시기 바랍니다.
제가 배우기로는 indigo는 푸른 식물성 색소이고 carmine은 붉은 동물성 색소(red coloring agent from eggs of female cochinea, a tropical insect from Mexico)입니다. 이를 섞은 것이 indigo carmine이라고 배웠습니다. 그런데 최근 Wikipedia등을 찾아보니 indigo dye의 sulfonated form을 indigo carmine이라고 부르며 Saxon blue와 같은 말이었습니다. 정식 명칭은 5,5'-indigotindisulfonate sodium이며 구조식은 C16H8N2Na2O8S2입니다 (참조: NCBI PubChem). pH 11.4에서 푸른색으로 pH 13에서 노란색으로 변하는 특징이 있어서 pH indicator로 사용된다고 하였습니다.
이름도 명확하지 않습니다. Ingido carmine, indigocarmine (띄어 쓰기 없음), indigo-carmine (hyphen 있음), Indigo Carmine (띄어 쓰기 있고 대문자) 중 어떤 것이 옳은지 모르겠습니다. 보통 indigo carmine (띄어 쓰기 있고 소문자이고 hyphen 없음)이라고 씁니다. 아마 이게 맞을 것입니다.
의학에서 indigo carmine의 용도는 다양합니다. 과거에는 renal function test 용으로 종종 사용되었습니다. 부작용으로는 bradycardia, hypertension, bronchospasm, urticaria 등이 가능한데 주로 정맥주사에서 나타납니다. 위내시경시 분무하여 나타나는 것 같지는 않습니다. 그러나 주의해서 나쁠 것은 없습니다. 생각컨데 ESD를 하면서 다량 사용하면 부작용이 나타날지 모릅니다. 그러나 실제 보고된 것을 보지는 못했습니다.
과거 (2010년 전후) indigo carmine은 공급이 불안정하여 간혹 재고가 바닥나는 경우가 있었습니다. 그럴 때마다 methylene blue를 대신 사용했습니다. 이가 없으면 잇몸입니다. 최근에는 비교적 안정적으로 공급되는 것 같습니다.
[Granules of indigo carmine]
Indigo carmine을 희석하여 사용할 때 잘 섞지 않으면 granule이 뭉친 상태로 뿌려집니다. 그럭저럭 병소를 살필 수 있지만 깨끗한 사진을 얻을 수 없습니다. 주사기를 다시 흔들어도 뭉친 granule이 잘 풀리지 않습니다. 아깝지만 버릴 수 밖에 없는 일입니다.
 5-2. Indigo carmine for gastric adenoma and cancer
5-2. Indigo carmine for gastric adenoma and cancer
Indigo carmine은 점막표면의 요철을 강조하는 색소입니다. 그래서 아래 사진과 같이 위암의 진단과 상세한 평가에 유용합니다.
선종이나 위암의 내시경 치료 전 indigo carmine은 꼭 사용하고 있습니다. 색소 살포 후 생각보다 병소가 커서 깜짝 놀라기도 합니다.

가운데 사진을 보십시오. 뚜렷하게 융기된 곳보다 원위부쪽으로 넓은 병소가 보였습다.
Stomach, ESD: Tubular adenoma with low grade dysplasia
1. Location : antrum, lesser curvature
2. Gross type : elevated
3. Size of adenoma : (1) longest diameter, 36 mm (2) vertical diameter, 31 mm
4. Resection margin : negative resection margins(N)
경계가 불분명한 위암의 내시경 치료였습니다. Indigo carmine이 매우 유용하였습니다.
Stomach, ESD: Early gastric carcinoma
1. Location : antrum, lesser curvature
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 30 mm (2) vertical diameter, 7 mm
6. Depth of invasion : invades mucosa (lamina propria) (pT1a)
7. Resection margin : free from carcinoma(N), safety margin : distal 15 mm, proximal 8 mm, anterior 6 mm, posterior 6 mm, deep 350 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Pre-existing adenoma : none
12. Microscopic ulcer : absent
13. Histologic heterogeneity: absent
14. Associated finding: Gastritis cystica superficialis
Indigo carmine은 요철이 없는 병소에서는 오히려 나쁠 수 있습니다. 아래 사진은 EGC IIb인데 indigo carmine을 뿌린 후 오히려 잘 보이지 않았습니다. 이럴 때는 irrigation을 해야만 다시 상세한 관찰을 할 수 있습니다.
 5-3. Bleeding by spraying indigo carmine solution
5-3. Bleeding by spraying indigo carmine solution
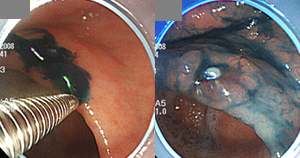
Indigo carmine 용액은 sprayer를 이용하여 뿌리는 경우가 많습니다. 간혹 너무 강하게 분무되어 병소에서 출혈이 발생합니다. 잘 보기 위하여 색소를 뿌렸는데 오히려 잘 보이지 않게 되었으니 낭패가 아닐 수 없습니다. 적당히 천천히 분무하는 수 밖에 없습니다.
저는 이런 경우를 막기 위하여 sprayer를 쓰지 않고 주사기를 이용하여 내시경 working channel로 직접 indigo carmine 액을 주입합니다. 내시경 working channel이 가득찬 후에야 indigo carmine 액이 분무됩니다. 따라서 10 ml 주사기를 쓰면 처음에는 거의 나오는 것이 없습니다. 다시 같은 주사기로 공기를 주입하면 그때서야 indigo carmine 액이 쫙~~~ 뿌려집니다. Sprayer 보다 압력이 낮으므로 출혈이 발생하지 않습니다.
저와 같이 약간 무식한 방법(무식해 보이지만 매우 좋은 방법입니다)을 쓸 때에는 한 가지 주의점이 있습니다. Dye를 다 뿌린 후 즉시 saline을 10 ml 정도 넣어주십시오. 그렇지 않으면 forcep이나 knife를 넣고 뺄 때 dye가 사방으로 튀게 됩니다.
 5-4. Is rountine spraying of indigo carmine helpful?
5-4. Is rountine spraying of indigo carmine helpful?
White light endoscopy에서 암이나 선종이 발견되면 indigo carmine을 분무하고 관찰합니다. 물론 상당히 도움이 됩니다. 그렇다면 white light endoscopy에서 특별한 이상이 없었던 경우 indigo carmine을 분무하면 어떨까요?
일본의 몇몇 내시경실에서는 상부위장관 내시경 도중 routine으로 indigo carmine을 뿌린다고 합니다. 그러나 routine chromoendoscopy가 도움이 된다는 증거는 거의 없습니다. 제가 하부위장관과 상부위장관에 대하여 각각 연구한 바 있습니다. 하부 위장관에서는 그나마 tiny adenoma가 몇 개 발견되었습니다. 그러나 상부위장관에서는 전혀 도움되지 않는다는 결과를 얻었습니다.
아직까지는 white light endoscopy로 자세히 보는 것이 최선이라고 생각합니다. 나무보다 숲을 보는 것이 중요하기 때문일 것입니다.
 6. Acetic acid for GI chromoendoscopy
6. Acetic acid for GI chromoendoscopy
Acetic acid는 pKa 4.8의 약산성으로 가장 작은 지방산(smallest of the fatty acids)입니다. 액체상태의 glacial acetic acid를 희석하여 사용합니다.
Acetic acid는 수십년 전부터 uterine cervix의 squamous columnar junction을 관찰하기 위하여 colposcopy에서 사용되어 왔습니다. 최근에는 위장관내시경에서도 간혹 사용됩니다. 산부인과 영역에서는 3-5% 용액을, 위장관내시경에서는 1-3% 용액을 사용합니다.
Unbuffered acetic acid가 상피세포를 만나면 일시적으로 상피세포 단백구조를 변화시킵니다. Squamous epithelium은 하얗게 변하고 columnar epithelium은 붉게 부어오르면서 표면구조가 강조됩니다. 바렛식도, 장상피화생 및 이형성의 관찰에 도움이 된다고 알려져있지만 (Rey. Endoscopy 2005) 실제 임상에서 사용되는 경우는 거의 없습니다. 저도 예를 보여드리지 못합니다. 사용 경험이 없기 때문입니다. 대장 쪽에서는 종종 사용된다고 합니다.
@ EndoTODAY가 나간 후 여러 선생님으로부터 연락이 왔습니다. Acetic acid를 상부위장관에서 사용하는 병원이 많은데 너무 소홀이 다루어졌다는 지적이었습니다. 감사합니다.
Methylene blue는 methylthionine chloride 용액을 지칭하는 용어입니다. 보통 0.5-1 % 용액을 분무하고 1-2분 기다린 후 물로 씻고 관찰합니다. 그러면 intestinal metaplasia 부위가 푸른색으로 염색됩니다. 특이하게도 gastric metaplasia는 염색되지 않습니다.
Methylene blue를 다량 사용하면 소변이나 대변이 푸른 색으로 변할 수 있으므로 놀라지 마십시오.
아래 사진은 intestinal metaplasia에 methylene blue를 뿌린 후 변화를 보여주고 있습니다 (물론 잠시 기다린 후 물로 씻었습니다). 그러나 실제 임상에서 intestinal metaplasia를 확인하기 위하여 methylene blue를 사용할 필요는 없다고 봅니다. (1) White light endoscopy를 이용해도 충분히 관찰할 수 있기 때문입니다. (2) Metaplastic gastritis로 진단한들 (간혹 검진 간격을 조절하는 것 이외에) 특별히 달라지는 것도 없기 때문입니다.
최근 저는 methylene blue를 거의 사용하지 않고 있습니다. 물론 교과서에서는 바렛식도에서 methylene blue가 유용하다고 되어 있습니다. 그러나 제가 경험한 바렛식도들은 white light endoscopy로 충분히 잘 보였으며, NBI를 쓰면 더할 나위 없이 명확해졌습니다. 도무지 색소가 필요하다는 생각이 들지 않았습니다.
다음에 말씀드릴 indigo carmine은 공급이 불안정한 색소입니다. 간혹 indigo carmine이 떨어질 때가 있다는 말씀입니다. 이럴 때 대용으로 methylene blue를 쓸 수 있습니다. 이것이 현재 저에게는 methylene blue의 유일한 용도입니다. 즉 indigo carmine 대용 정도의 가치가 전부인 셈입니다.
[2018-9-19. 애독자 질문]
저는 로컬에서 근무하는 소화기의사인데 최근 인디고카민 공급에 차질이 생겼는지 공급이 안된다고 하더라구요. 과거에 포스팅하신 글 중에 인디고카민 대신 메틸렌블루를 대체재로 사용하신다고 하셨는데 그 사용목적이 점막상태를 평가하기위한 도포용인지 아니면 그 외에 대장용종 제거를 위해 injection도 가능한 건지에 대해 궁금해서 메일드립니다. 그리고 또 다른 대체재 약물이 있는지 알려주시면 감사하겠습니다.
[2018-9-22. 이준행 답변]
왜 공급에 차질이 있는지 저는 잘 모르겠습니다. 저희 병원에서는 아래 제품을 쓰고 있는데 아직까지는 별 문제가 없습니다.
인디고카민 대신 메틸렌블루를 사용하기도 한 적이 있습니다. 요철을 보기 위한 용도였습니다. 그러나 아시다시피 인디고카민은 흡수되지 않는 약이고 메틸렌블루는 흡수되는 것이므로 대체하는 약은 아니고 그냥 임시방편이었들 뿐입니다. 인디고카민을 대신할 수 있는 좋은 alternative는 아직 없는 것 같습니다.
[2022-2-25] 알림 indocyanine green/ 재고에 대하여
현재 수술 전 tattoo를 위하여 사용되고 있는 indocyanine green이 제조사 사정으로 장기 품절될 것이라고 합니다. 현재 재고를 아껴쓰고 있으며 하루 빨리 상황이 호전되기를 기도합니다. 할 수 있는 것이 기도밖에 없습니다.
[2022-3-18] Indocyanine green이 한국희귀필수의약품센터에서 공급된다고 합니다. 휴~~~
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.