 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [위매독. Gastric syphilis] - 終
[위매독. Gastric syphilis] - 終
1. 위매독의 임상적 특징 Clinical features of gastric syphilis
2. 위매독의 내시경 소견 Endoscopic findings of gastric syphilis
3. CPC case
4. More cases
6. References
최근 위매독(gastric syphilis)이 조금씩 증가하는 것 같다는 의견입니다. 전체적으로 매독이 증가하고 있으므로 위매독도 따라서 증가하는 것 아닐까 싶습니다. 우리나라에서 매독 환자는 생각보다 많습니다. 2008년의 경우 1,548명이었다고 합니다 (Clin Endosc 2015;48:256). AIDS로 인해 다른 성병이 무시되고 있기 때문인 것으로 추정됩니다.
Gastric syphilis의 특징을 정리하면 아래와 같습니다.
1. Secondary and tertiary stage
2. Incidence in syphilis; <1%
3. Endoscopy; erosive gastritis or gastric ulcer with heaped, nodular edges or thickened, edematous rugal folds.
4. Histopathologic findings; suggestive, but not diagnostic
제가 지금까지 알고 있는 gastric syphilis 6예의 사진입니다. 특히 첫번째 증례는 보만 4형 진행성 위암과 비슷하다고 의뢰되었던 경우입니다.
2020-2-1. 부산경남지회 심포지엄. 좋은삼성병원 이태영
History: A 25-year-old, apparently healthy man presented with one month history of epigastric tenderness and vomiting. The patient visited a local clinic where he underwent an endoscopic examination and the endoscopic diagnosis was benign gastric ulcer. But gastric ulcer symptom was not improved on ulcer medication. He was transferred to our hospital for further evaluation. His family history and past medical history were negative for any gastrointestinal disease, abdominal surgery or significant medical illness. Physical examinations were normal except minimal epigastric tenderness only. A laboratory evaluation revealed hemoglobin of 16.4 g/dL and hematocrit 47.9%. White blood cell count and differential count were within normal ranges. Total serum protein level was 7.3 g/dL and albumin level 4.3 g/dL. Serum bilirubin and liver enzymes were within normal ranges. A computed tomographic scan of the abdomen with contrast revealed diffuse layered thickening of the wall of the gastric antrum, pylorus, duodenal bulb, and second portion of duodenal loop without definite perigastric and periduodenal fatty infiltration (Fig. 1). Multiple small and enlarged lymph nodes were identified along both common femoral vessel and inguinal area. Gastric endoscopy showed geographic irregular ulcer and shallow depressed mucosal lesions in almost all aspect of the antrum. The ulcer revealed an irregular edge and uneven nodular base (Fig. 2). Endoscope was failed to advance to the duodenal bulb due to luminal obstruction. A diagnostic procedure was done.
Biopsy: Chronic gastritis, active, with intestinal metaplasia (incomplete type), large lymphoid follicle and dense lymphoplasma cell infiltration ( Note: Based on histology, syphilitic gastritis could be considered)
Layered wall thickening involving gastric antrum, pylorus, duodenal bulb,and 2nd duodenal loop
Automated Quantitative RPR Test: Reactive(5.00)
Automated Quantitative TPLA Test: Reactive(282.9)
A: foveolar pit 에서 H.pylori 가 관찰되지 않는다. B: 심한 위염소견으로 neutrophilic infiltration 이 관찰된다. C: lamina propria 에 심한 lymphoplasma cell infiltration 이 관찰된다. D: lagre irregular lymphoid follicular hyperplasia with geographic feature
Large irregular lymphoid follicle : H.pylori 감염과는 달리 marginal zone 은 상대적으로 위축되어 있으나 follicular center 가 심하게 늘어나면서 지도모양(geographic feature) 으로 커져있다.
CPC에서 논의되었던 이 환자는 증례보고를 하였습니다 (위와 십이지장을 침범한 매독 1예).
 4. More cases of gastric syphilis
4. More cases of gastric syphilis
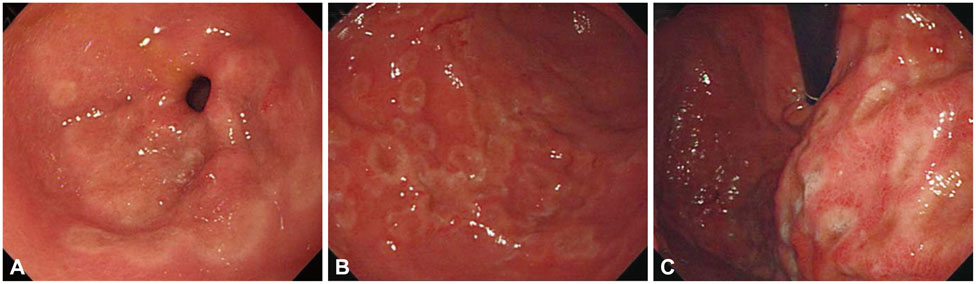
신증후군을 동반한 위매독 (Clin Endosc 2015). Gastroscopic findings. Multiple irregular, shallow ulcers covered with whitish exudates and central depression in the (A) antrum, (B) body, and (C) cardia. Histologic findings of gastric biopsy. (A) Marked severe inflammation with lymphoplasmacytic infiltrates (H&E stain, ×400). (B) Numerous spirochetes are present between foveolar epithelial cells (Warthin-Starry stain, ×1,000).
41세 러시아 국적 남성의 대장내시경에서 발견된 직장 매독 증례를 소개합니다 (Korean J Gastroenterol 2016).
논문에 언급된 병력과 검사 소견을 옮깁니다.
"내원 한 달 전 항문 성교를 한 경험이 있었으며 내원 2주 전에 항문 주변에 통증이 있었다고 하였다. 직장 내 궤양 병변에 대한 감별 진단을 위해 추가 검사를 시행하였으며 혈청 매독균 특이항체(syphilis specific Ab) 검사에서 양성, 비트레포네마 검사(nontreponemal test) 결과 반응성 소견이 관찰되었다. 인간면역결핍바이러스(human immunodeficiency virus) 항체 및 항원 검사는 모두 음성이었다. 항문연 상방 부위의 궤양 병변에서 시행한 조직검사 결과는 궤양과 육아조직을 동반한 직장염 소견이었으며(Fig. 3), 추가로 시행한 Warthin-Starry 염색에서 스피로헤타(Spirochaete) 소견이 관찰되어 매독으로 진단할 수 있었다(Fig. 3B). 환자는 매독 치료를 위해 doxycycline 복용을 시작하였으며 추적 관찰은 연고지 병원에서 시행하기로 하였다."
1) Gastric syphilis: a systematic review of published cases of the last 50 years. Sex Transm Dis 2010
The authors conducted a systematic review of the English literature for cases of Gastric Syphilis (GS) in the last 50 years. The 34 studies which met selection criteria included 52 patients with GS. Of the reviewed patients, only 13% had a history of syphilis diagnosis and 46% had prior or concurrent clinical manifestations of the disease. Epigastric pain/fullness was the most common presenting symptom (92%) and epigastric tenderness being the most common sign. Gastric bleeding of variable intensity was documented in 35% of the cases. In the radiologic examinations, fibrotic narrowing and rigidity of the gastric wall was the most common finding (43%), followed by hypertrophic and irregular folds, while in endoscopy the most common lesion types were multiple ulcerations (48%), nodular mucosa, and erosions. The antrum was the most commonly affected area (56%). The majority of the patients received penicillin (83%) with a rapid resolution of their symptoms. Seventeen percent of the patients were treated surgically either due to a complication or due to strong suspicion of infiltrating tumor or lymphoma. The nonspecific clinical, radiologic, and pathologic characteristics of GS can establish it as a great imitator of other gastric diseases. GS should be considered in the differential diagnosis in patients at risk for sexually transmitted diseases who present with abdominal complaints and unusual endoscopic lesions and no other diagnosis is made, irrespective of the presence of H. pylori. The absence of primary or secondary luetic lesions should not deter one from considering GS.
2) Syphilis: A Review JAMA 2025
Importance: Syphilis is an infectious disease caused by Treponema pallidum, a gram-negative, spirochete bacterium. Worldwide, an estimated 8 million adults aged 18 to 49 years acquired syphilis in 2022. From 2019 to 2023, US syphilis cases increased by 61% overall, with diagnoses among females increasing by 112% and congenital syphilis cases increasing by 106%.
Observations: Syphilis is transmitted via contact with infectious lesions during vaginal, anal, or oral sex or via the placenta during pregnancy. Individuals at increased risk for syphilis include people with HIV, those engaging in condomless sex with multiple partners, and men who have sex with men (MSM)-who comprised one-third (32.7%) of all males with primary and secondary syphilis in 2023. Early syphilis is defined as syphilis in the first year after infection and includes symptomatic (primary and secondary) and asymptomatic (early latent) stages. Primary syphilis is characterized by painless anogenital lesions. Secondary syphilis is associated with a diffuse rash, mucocutaneous lesions, and lymphadenopathy. Syphilis diagnosed more than a year after infection is referred to as late syphilis and includes asymptomatic (late latent) and symptomatic (tertiary) stages. Neurosyphilis, which can occur at any stage, can lead to meningitis, uveitis, hearing loss, or stroke. In pregnancy, up to 40% of fetuses with in-utero exposure to syphilis are stillborn or die from their infection during infancy. The diagnosis of syphilis relies on serologic reactivity along with a clinical history and presentation consistent with active or latent syphilis infection. The recommended treatment for syphilis is benzathine penicillin G administered as intramuscular doses of 2.4 million units: a single injection for early stage and 3 weekly injections for late latent stage syphilis. Strategies to identify and prevent syphilis infections include (1) screening of sexually active people aged 15 to 44 years at least once and at least annually for those at increased risk, (2) screening 3 times in pregnant individuals (at the first prenatal visit, during the third trimester, and at delivery), (3) counseling about condom use, and (4) offering doxycycline postexposure prophylaxis (200-mg doxycycline taken within 72 hours after sex as postexposure prophylaxis) to MSM and transgender women with a history of a sexually transmitted infection in the past year.
Conclusions and relevance: Syphilis infections, including congenital syphilis, have increased in the US and worldwide over the past decade. First-line treatment for syphilis is benzathine penicillin G. Routine syphilis screening of all pregnant patients and all sexually active people aged 15 to 44 years and use of doxycycline postexposure prophylaxis in individuals at risk for syphilis infection are recommended strategies to decrease syphilis transmission.3) [연합뉴스] 국내서 늘어난 '매독'…증상과 치료법은?

4) [YTN] 증가하는 성매개감염병, 매독과 헤르페스

© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.