 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [생선뼈 이외의 식도 이물. Esophageal foreign body other than fish bone] - 終
[생선뼈 이외의 식도 이물. Esophageal foreign body other than fish bone] - 終
2. In patients without stricture
3. Shell
4. PTP press through pack
5. 실리카겔 플라스틱 튜브
7. Sedation during foreign body removal
9. Complication - acute mediastinitis
10. Cases
11. References
식도 협착을 가진 환자는 작은 음식 조각도 걸릴 수 있습니다. 식도암 수술 후 문합부에 마늘이 걸려 내원한 예입니다. 음식이 걸리면 물도 안 넘어가게 됩니다.
Lye stricture를 가진 환자에서 식도 이물이 반복되기 쉽습니다. 생선매운탕 드신 후 생선 눈알이 협착부에 걸렸던 예입니다.
땅콩
 2. In patients without stricture
2. In patients without stricture
갈비. 식도 협착이 없는 환자에서도 다양한 음식이 걸릴 수 있습니다. 70대 환자가 갈비를 드시다 식도위접합부에 걸린 예입니다. 천천히 잘 씹어 드세요. Slow food 운동이라도 해야겠습니다.
알약
돼지고기 물렁뼈
파인애플
플라스틱 재질 치과용 crown
특별한 organic disease가 없는 분인데 식도의 second physiologic narrowing에 음식물 덩어리가 걸려있어서 net로 제거하였습니다.
특별한 organic disease가 없는데 esophageal food impaction이 발생하면 조직검사를 해 보면 좋을 것 같습니다. 2015년 11월 Digestive Diseases Sciences에 실린 메타분석(Hiremath GS. Dig Dis Sci 2015)에 따르면 esophageal food impaction으로 조직검사한 사람의 절반이상이 eosinophilic esophagitis로 진단된다고 합니다.
조개껍질은 식도 협착이 없어도 종종 걸립니다.
조개국물 빨리 마시지 마세요. 실수하면 껍질이 넘어갑니다.
[2022년 설연휴 식도이물제거술 Instagram]
인스타그램에서 가져온 사진입니다. 코로나와 연휴로 인하여 어렵게 어렵게 식도이물제거술이 시행된 모양입니다. 고생하셨습니다.
PTP를 그대로 삼켜 응급실로 오시는 환자가 있습니다. 이유는 다양합니다. 고령환자가 많습니다. 잠결에 혹은 급하게 약을 먹다가 실수하는 수도 있습니다. 내시경으로 PTP를 제거할 때에는 식도벽 손상에 주의해야 합니다. Cap을 사용하는 것이 좋습니다.
Overtube를 사용하면 나올 때 상부식도 손상을 줄일 수 있겠지만, overtube를 넣은 과정에서 PTP로 인한 식도 손상을 악화시킬 수 있습니다. 가급적 overtube를 사용하지 말 것을 권합니다.
PTP 제거 전 CT를 찍어 천공이 없는지 확인하는 것이 안전합니다. 내시경으로 PTP를 제거한 후에는 다시 내시경을 삽입하여 천공과 같은 합병증이 없는지 살피기 바랍니다. 필요하면 clipping을 시행하고 항생제를 사용합니다.
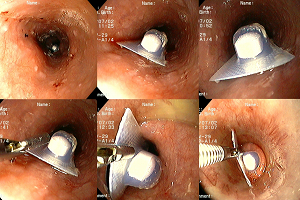

Cap을 장착한 내시경을 사용하여 alligator를 이용하여 제거하였고 상부식도의 linear laceration이 있었으나 특이 치료 없이 호전됨.
[증례] 식도이물 (PTP; press through pack)로 외부에서 외부에서 이물제거술을 시행받았으나 실패한 상태로 의뢰되었던 분입니다. 외부 CT에서부터 extraesophageal air가 있어서 천공된 상태였습니다. 내시경으로 조심스럽게 PTP를 위로 밀어넣은 후 surgical grove parachute 방법으로 제거할 수 있었습니다. 처음 PPT가 걸렸던 자리에 천공이 관찰되었기 때문에 clipping으로 치료하였습니다.
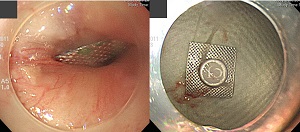
60대초반 여성이 PTP 포장약품(proton pump inhibitor)을 낱개로 절단해서 포장채 복용 후 흉부불편으로 오셨는데, 식도 중간부위에 걸려 있었습니다. 다른 약들과 함께 복용하기 쉽게 PTP 약을 하나씩 절취해 두었는데 생각없이 함께 복용하였다고 합니다.
몇번째 경험하는 식도손상 안전사고인데, 고령화 시대에 더 빈발 할 것입니다. 복약지도나 안전문구로만 부족할 것같습니다. 저는 대안으로 입에 들어가지 못할 크기로 PTP포장을 만들어도 좋을 듯합니다. 사고가 난 약(좌측)의 PTP 포장은 2 x 2 cm인데 반하여, 당뇨약 콤비글라즈(우측)는 3.5 x 5 cm으로 절대 입에 못 들어갈 크기입니다.
[2014-12-29. 이준행 답변]
좋은 증례 감사합니다. 저도 몇 번 경험하였습니다. 제 경우에는 사각형 약봉지에 PTP 약을 함께 포장해서 환자가 무심결에 함께 먹었던 경우가 많았습니다. 조제오류인 셈이었습니다. 설마 약사님들이 이런 실수는 하지 않을 것이므로, 누군가 대신 포장한 것을 제대로 점검하지 못하였던 경우였을 것으로 막연히 추측하였습니다. 선생님 아이디어처럼 PTP를 5 cm로 만들어 절대로 못 삼키게 하는 것도 좋은 방법일 것 같습니다.
시대가 달라지면 이물도 달라집니다. 비타민 알약을 먹다가 실리카겔이 담긴 플라스틱 통을 함께 먹고 이물감으로 내원환 환자입니다. CT에서 매우 하얀 이물이 보였습니다. 지금까지 보았던 이물 중 CT에서 가장 하얗게 보인 이물입니다 (노란색 화살표). 실리카겔의 주성분이 이산화규소입니다. 규소가 주기율상 알루미늄이나 칼슘 엇비슷한 경금속에 해당하니 그 정도 opacity가 나오는 모양입니다. 참고로 철분제제 먹고 엑스레이 찍으면 뱃속에서 알약이 보인다고 합니다 (자문교수: 영상의학과 정명진).
오른쪽 위 작은 사진이 내시경으로 꺼낸 이물입니다. 언끗 알약과 구분되지 않는 모양으로 실리카겔 통을 디자인한 사람은 안전에 대한 개념이 전혀 없다고 할 수 있습니다. 디자인부터 안전해야 합니다.
식도에 뭔가 걸리면 금방 병원에 올 것이라고 생각하기 쉽습니다. 그러나 천천히 오시는 분도 계십니다. 닭뼈가 목에 걸렸는데 4일만에 병원을 찾으신 분입니다. 식도 방향의 직각으로 뼈가 걸려있었고 내시경으로 제거할 수 없어서 이비인후과에 의뢰하여 rigid esophagoscope로 제거한 예입니다.
낚시 바늘이 목에 걸렸는데 2달만에 병원을 방문한 환자도 있었습니다. 폐암 환자였습니다. 놀랐습니다.
어느 날 바닷가 식당에서 생선을 먹다가 낚시 바늘을 발견했습니다. 식당 주인에게 약간의 항의를 하려고 보여주었는데, 식당 주인은 "자연산이라는 확실한 증거입니다. 우리 집은 자연산만 씁니다."라고 말했습니다. 전혀 사과하는 기색이 없었습니다.^^
의료접근성이 떨어지는 해외에서 거주하기 때문이었지만 PTP가 몇 주 걸려있던 환자도 있었습니다.
 7. Sedation during foreign body removal
7. Sedation during foreign body removal
식도 이물제거술 도중 upper esophageal sphincter(UES)에 걸려서 나오지 않는 경우가 있습니다. 저는 midazolam을 사용하여 도움을 받은 적이 있습니다.
PEG tube change 도중 잘려진 internal bumper가 UES에 걸려 빼낼 수가 없었습니다. 환자가 지나치게 힘을 주고 있었던 것이지요. Midazolam을 주사한 후 쉽게 제거할 수 있었습니다.
식도 이물에는 합병증이 따릅니다. 내시경 제거술 후 합병증도 가능하지만 오늘의 증례처럼 처음부터 천공된 상태로 응급실을 찾기도 합니다.
 9. Complication - acute mediastinitis
9. Complication - acute mediastinitis
Acute mediastinitis로 내원하신 분으로 병력상 생선가시가 걸렸다가 저절로 풀린 적이 있었습니다. 내시경을 하였을 때에는 식도에 이물이 관찰되지 않았지만, 다른 원인이 없었으므로 식도이물 합병증으로 추정하였습니다.
식도이물로 환자가 사망할 수도 있습니다. Fatal empyema 증례 보고도 있습니다 (Korean J Gastrointest Endosc 2007;34:320-323).
소의 양(stomach)이 상부식도에 걸려 이물제거술을 하였고 수일 후 추적검사에서 식도암이 발견되어 의뢰된 환자로 수술 (Ivor-Lewis and 3 field dissection) 후 adjuvant chemotherapy를 받았고 11년 간 재발 소견 없었음.
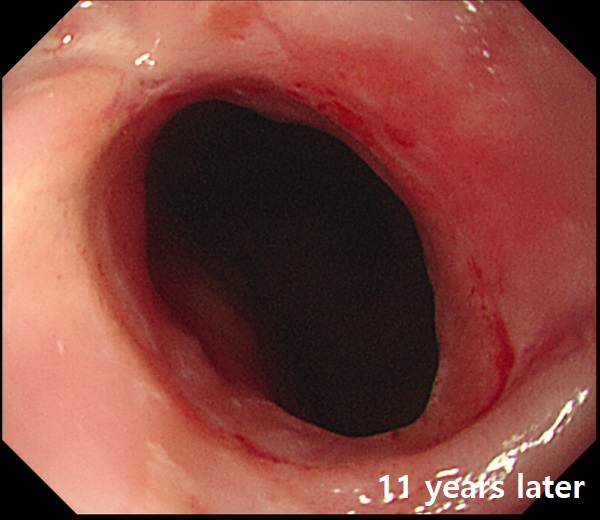
Esophagus and upper stomach, Ivor Lewis operation: Invasive squamous cell carcinoma, moderately differentiated, proximal esophagus:
1) tumor size: 3.5x3 cm
2) extension to submucosa
3) endolymphatic tumor emboli: present
4) perineural invasion: not identified
5) negative but very close to proximal resection margins
6) metastasis to 2 out of 78 regional lymph nodes (2/78: "RRLN", 0/1; "LRLN", 1/4; "RD", 0/4; "LD", 0/0; "LC1", 0/0; "8U", 0/1; "7", 0/7; "RT.LEVEL 3", 0/5; "RT.LEVEL 4-5", 1/7; "R9", 0/2; "LT.LEVEL 3", 0/8; "LT.LEVEL 4-5", 0/7; "LEVEL 6", 0/11; "L9", 0/1; "L10", 0/1; "G1", 0/5; "G2", 0/1; "G3", 0/13)
7) no tumor, "lesser curvature omentum" and "EG junction"
음식물이 식도에 걸려 내시경 식도이물제거술 후 식도암 발견. CCRT 및 수술로 치료하였으나 결국 식도암의 위전이가 발견되었음
순간접착제를 드셔서 인후부, 식도 및 위에 corrosive injury가 있던 분입니다. 식도와 위 내강에서 순간접착제가 굳어서 하얗고 길쭉한 foreign body가 만들어진 것 같습니다.
돼지뼈가 걸려서 천공. 이비인후과에서 rigid esophagoscope로 제거
원인미상의 식도천공으로 오셨는데 닭을 드신 후 증상이 발생하였기 때문에 닭뼈에 의한 천공으로 추정하였음. 내시경은 증상 발생 1주일 후 시행됨.
* 참고: 기도를 압박하여 호흡곤란을 유발한 식도이물 1례 (PDF, 0.2M)
1) EndoTODAY 이물
2) 소아 식도 이물 (battery) - 내시경학회 교육자료 (2016/7)
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.