 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [위암의 깊이. Depth of invasion of gastric cancer (침윤 깊이. 심달도)] - 終
[위암의 깊이. Depth of invasion of gastric cancer (침윤 깊이. 심달도)] - 終
심달도(深達度)는 일본식 표현이므로 가급적 '침윤 깊이'라는 표현을 사용하시기 바랍니다.
1. 조기위암과 진행성위암의 구분 - 병리학적 기준
6. 보만 1형 진행성 위암과 EGC type I의 구분
7. Cases
8. FAQs
9. References
위암의 깊이에 대한 내시경 평가의 정확성에 대한 논문은 객관적이기 어렵습니다. 관찰자간 차이가 크기 때문입니다. 일본과 우리나라의 결과도 제법 다릅니다. 우리는 우리 실정에 맞는 데이타를 참고하여 환자진료에 응용하는 것이 좋을 것입니다. 2011년 서울대학교병원에서 위암 깊이 평가의 정확성에 대한 논문을 낸 바 있는데 우리 현실을 잘 보여주는 좋은 참고자료라고 생각합니다 (최정민. GIE 2011).
조기위암에서 진행성위암으로 변하는 기간은 연구하기 어렵습니다. 일본의 한 연구에서는 44개월을 제시한 바 있습니다 (Tsukuma H. Stomach Intestine 2008:43:1777-83). 같은 연구에서 5년 후 64.7%, 10년 후 95% 이상이 진행성위암으로 발전한다고 합니다.
2010년 삼성서울병원 외과의 분석(Shin SH. J Surg Oncol 2010)에 따르면, 내시경에서 조기위암으로 추정하였던 1,611명 중 120명(7.4%)이 진행성위암이었습니다. 내시경치료를 하였던 조기위암이 포함되었더라면 약간 더 좋았을 것입니다. 내시경에서 진행성 위암으로 추정하였던 1,299명 중 132명(10.2%)은 조기위암이었습니다. 일반적으로 내시경에서 조기위암으로 생각한 위암의 5%는 진행성 위암, 내시경에서 진행성위암으로 생각한 위암의 10%는 조기위암으로 생각하기 바랍니다.
2011년 서울대병원 논문 (최정민. GIE)에서 내시경으로 조기위암으로 추정된 2,105명 중 2.9%인 60명은 실제로는 진행성위암이었습니다. 이 정도의 정확도는 매우 우수한 것입니다.
2013년 건국대 논문 (Clin Endosc)에서 조기위암으로 추정된 207명 중 6.8%인 14명은 실제로는 진행성 위암이었습니다. Proximal part에 EGC-like AGC가 많았습니다.
AGC-like EGCs predominate in the distal part of the stomach, while EGC-like AGCs predominate in the proximal part. When evaluating the depth of a gastric cancer, care should be taken not to underestimate measurements in proximal gastric cancers since they tend to be poorly-differentiated adenocarcinomas, in Lauren’s diffuse type, and invade deeper than their endoscopic appearance might suggest.
2015년 한양대병원 논문에서 내시경에서 조기위암으로 판단하였던 367명 중 40명(11 %)이 진행성위암이었습니다 (Lee JH. Surg Endosc 2015 - Epub).
PM cancer는 조기위암과 진행성 위암의 중간적 성격을 가지고 있습니다. 제가 전공의 시절에 분석한 자료를 군대 기간동안 출판한 논문이 PM cancer에 대한 것이었습니다.
[조기 위암과 진행성 위암의 구분의 병리학적 기준]
암세포가 명백하게 proper muscle layer의 muscle 사이에 침윤하면 당연히 PM cancer입니다. 그러나 암세포가 명백히 muscle 조직을 침윤하지 않았지만 뚜렷하게 PM layer를 누르고 있으면 (= PM 상단을 연결한 가상의 선 아래까지 침윤된 경우) 병리학적으로는 PM cancer로 분류됩니다. 즉, 진행성 위암입니다. 그런데 일본의 일부 병리학자들은 이를 SM massive라고 부른다고 합니다. 즉, 조기위암으로 분류한다는 것입니다. 흥미로운 국가간 차이인데요, 여하튼 우리나라에서는 우리나라의 기준을 따라야 하겠지요.
육안소견으로 deep SM cancer를 의심하였는데 진행성 위암으로 보고되었습니다.
모처럼 병리 가이드라인이 update 되어 2023년 대한위암학회지(JGC)와 대한병리학회지(JPTM)에 동시 출판되었습니다. 해당 병리 가이드라인 중 위암 침윤 깊이 판정에 대한 내용을 소개합니다. Depth of invasion 판단과 T staging 결정은 생각만큼 간단하지 않습니다. Lymphatic vessel 내에 있는 것은 T staging에 반영하지 않는다는 부분도 유의하시기 바랍니다.
A standardized pathology report for gastric cancer: 2nd edition (Journal of Pathology and Translational Medicine 2023;57:1-27)
The depth of the tumor invasion follows the AJCC 8th edition and Japanese guidelines. Notably, the Japanese guideline does not accept carcinoma in situ (pTis). In the AJCC 8th edition, pTis is defined as an intraepithelial tumor without invasion of the lamina propria, which is equivalent to high-grade dysplasia. pT1b is subdivided into sm1, sm2, and sm3. If cancer cells are present below an imaginary line dividing the submucosa and proper muscle, the case is considered pT2 even if the cancer cells are not actually within the muscle fibers. If there is no proper muscle layer due to ulceration, and the cancer cells are below the imaginary line drawn at the lower border of the proper muscle, the case is considered pT3. Invasion of the omentum and perigastric fat is considered pT3. Ink should be applied at the serosal surface nearest the tumor during gross examination to properly evaluate serosal (visceral peritoneum) invasion. The case is considered pT4a if the cancer cells are adherent to or exposed beyond mesothelial cells. Because the mesocolon and gastric serosa (including the greater and lesser omentum) have different embryological origins, invasion of the mesocolon should be classified as pT4b. However, some areas are tightly fused, such as the posterior wall of the antrum, the gastric serosa, and the anterior side of the transverse mesocolon. Therefore, the Japanese guideline indicates that invasion of the transverse mesocolon is not pT4b unless it extends to the colic vessels or penetrates the posterior surface of the mesocolon. Some cases can be either pT4a or pT4b, depending on the site of the tumor. Invasion of the pancreas capsule is considered pT4b. Direct duodenal or esophageal invasion is not considered pT4b. Any involvement of other organs, such as the liver, pancreas, colon, spleen, diaphragm, or kidney, should be recorded. Cancer cells within lymphatic or vascular spaces are not considered in the determination of invasion depth. The presence of lymphatic or vascular invasion should be recorded separately in parentheses (e.g., tumor invades proper muscle [involvement of subserosa by lymphatic emboli]).
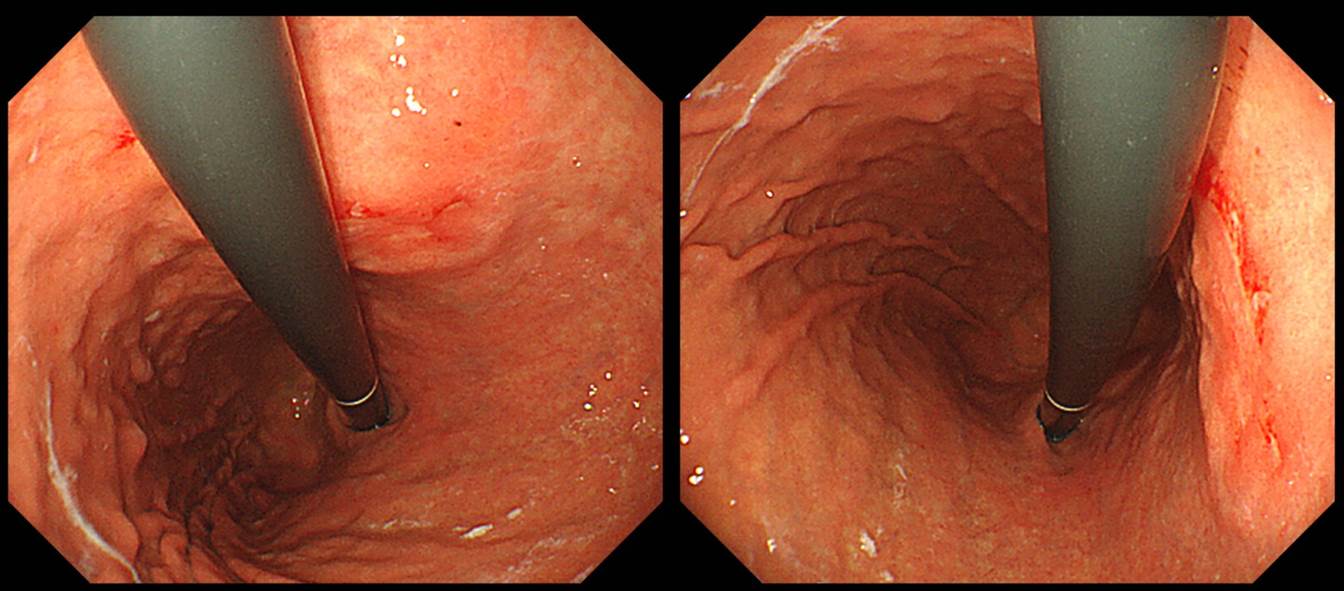
조기위암 깊이(depth of invasion) 평가의 중요한 요소 중 하나는 fold 변화입니다. Fold는 위내에 공기를 어느 정도 뺐을 때 잘 관찰됩니다. 공기를 약간씩 넣고 빼면서 병소 주변 점막의 변화를 조심스럽게 관찰하는 것이 좋습니다.
조기위암 fold에 대한 (간단하지만 그리 정확하지 않은) 대원칙은 다음과 같습니다. 점막암에서는 abrupt cutting, rapid tapering (= rat-tailing, 쥐 꼬리처럼 생겼다는 의미), 점막하암에서는 fusion, clubbing이, 고유근암(PM cancer)에서는 dam-formation이 관찰됩니다. Fold 변화는 위암 깊이 예측의 중심이지만 fold에 따른 깊이 진단이 꼭 옳은 것은 아닙니다. 깊이 예측은 예술입니다. EGC로 추정했는데 AGC로 나오는 경우는 약 5-10%입니다. AGC로 추정했는데 EGC로 나오는 경우도 약 5-10%입니다. (대한소화기내시경학회지 2007;35:297-303)
이번 증례는 (1) 함몰부가 비교적 깊고, (2) fold fusion 소견이 여럿 관찰되고, (3) 조직형이 signet ring cell carcinoma이었으므로 눈으로 보기보다 다소 깊을 수 있을 여지가 많았던 경우입니다. 비록 내시경에서 EGC III (r/o submucosal cancer)라는 impression을 붙일 수 밖에 없지만... 약간 깊다고 나왔지만 놀랄 필요는 없을 것 같습니다.
서울대 논문 (최정민. GIE)에서 점막암으로 추정된 1,276명 중 1,026명(82.0%)는 점막암이었고, 점막하암으로 추정된 829명 중 596명 (71.9%)는 점막하암이었습니다.
서울대 논문에서는 조기위암 침윤깊이 예측의 기준이 되는 여러 소견의 의미가 분석되어 있습니다. 너무 복잡하여 그 의미를 정확기 알기는 어렵습니다. 그러나 간단히 생각하면 이것입니다. "어느 한 소견으로 점막암과 점막하암을 구분할 수 없다."
서울대 논문에서 제가 흥미롭게 본 것은 단변량 분석과 다변량 분석의 차이입니다. 아래 표에서 좌측이 단변량 분석이고 우측이 다변량 분석입니다. 단변량 분석에서 undifferentiate-type histology는 differentiated-type histology에 비하여 침윤깊이 예측 정확도가 떨어집니다 (OR=0.804, p=0.046). 다변량 분석에서는 p 값 0.889 (OR=0983)로 차이가 없었습니다. 무엇때문에 단변량에서의 의미가 다변량에서는 사라졌는지 저로서는 알 도리가 없습니다.
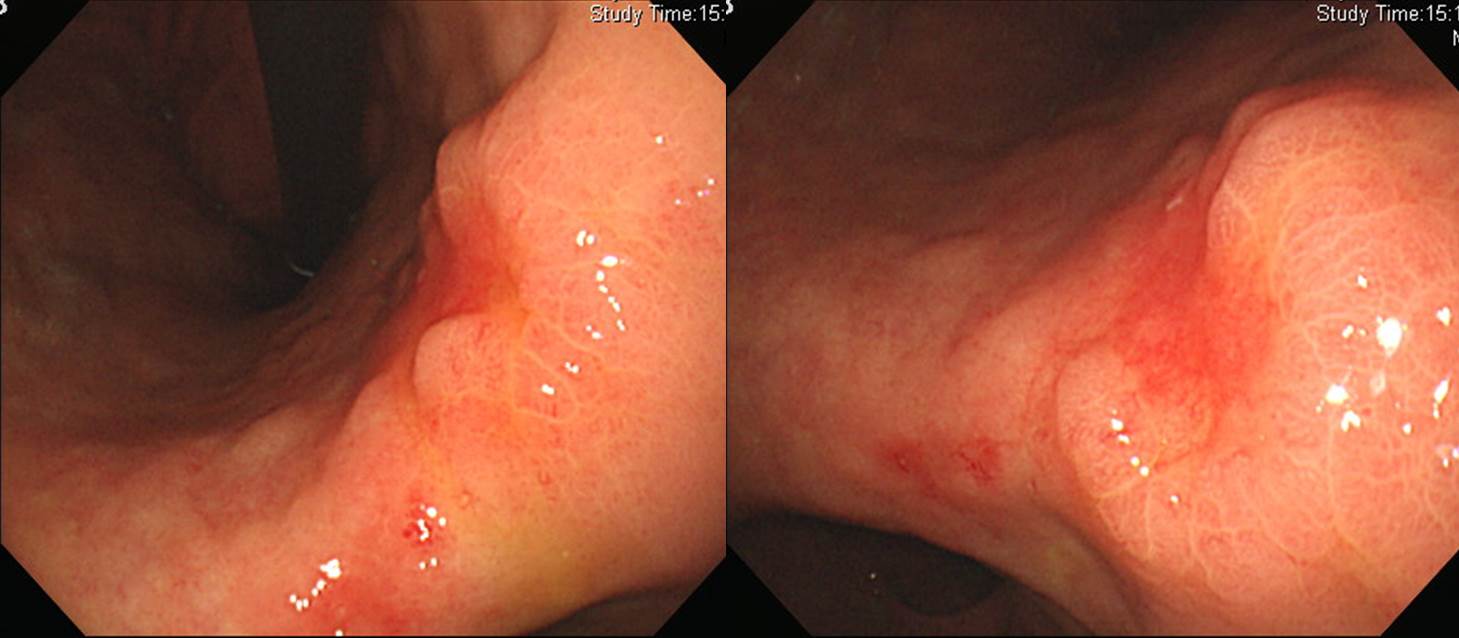
2023년 Surgical Endoscopy지에 조기위암 심달도 평가를 위한 conventional endoscopy와 EUS의 정확도에 대한 일본의 다기관 전향적 연구 결과가 발표되었습니다 (Surg Endosc 2023). SM2 이상의 점막하암 (massive submucosal invasion이라고 칭하기도 합니다)을 시사하는 소견으로 아래 사진이 제시되었습니다.
Clin Endosc 2015년 6월호에 실린 충남대 문희석 교수의 종설(Improving the Endoscopic Detection Rate...)에서 흥미로운 사진을 옮깁니다 (위암 294).
문교수님은 이렇게 쓰셨습니다. "Remarkable elevation of the tumor is seen with a converging fold. This findings fulfill the criteria for massive submucosal invasion by tumor." 일전에 differentiated-type EGC의 depth-predicting score를 소개한 바 있습니다 (Abe. Gastric Cancer 2011). 이 논문의 결론은 아래와 같았습니다.
On logistic regression analysis, tumor size more than 30 mm, remarkable redness, uneven surface, and margin elevation were significantly associated with deeper submucosal cancers. A depth-predicting score was created by assigning 2 points for margin elevation and tumor size more than 30 mm, and 1 point for each of the other endoscopic features. When validation lesions of 3 points or more were diagnosed as deeper submucosal cancers, the sensitivity, specificity, and accuracy as evaluated by three endoscopists were 29.7-45.9, 93.1-93.7, and 82.5-84.8%, respectively.
일본 저자가 말한 margin elevation과 문희석 교수님의 말씀은 약간 다르기는 합니다. 여하튼 함몰형 병소에서 공기를 약간 빼고 관찰하였을 때 전체적으로 융기된 병소는 massive submucosal invasion을 시사하는 소견입니다. 대장암에서는 이러한 특징이 보다 현저히 관찰됩니다.
점막하암으로 추정했는데 의외로 점막암이 나왔습니다. 심달도는 어렵습니다.
Stomach, Subtotal gastrectomy: Early gastric carcinoma
1. Location : middle third, Center at mid body and posterior wall
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : mixed
5. Size : 3.8x2.4 cm
6. Depth of invasion : invades mucosa (lamina propria) (pT1a)
7. Resection margin: free from carcinoma, safety margin: proximal 1.5 cm, distal 11.7 cm
8. Lymph node metastasis : no metastasis in 22 regional lymph nodes (pN0)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. AJCC stage by 8th edition: pT1a N0
조직검사에서 poorly differentiated로 나오는 경우는 육안소견보다 다소 깊은 경우가 많습니다. 우리가 침윤 깊이를 논하는 것은 분화 조직형 위암에 해당한다고 이해하는 것이 좋겠습니다.
Stomach, radical subtotal gastrectomy: Advanced gastric carcinoma
1. Location : middle third, Center at body and anterior wall
2. Gross type : Borrmann type 2
3. Histologic type : tubular adenocarcinoma, poorly (solid) differentiated
4. Histologic type by Lauren : diffuse
5. Size : 2.5x2.2 cm
6. Depth of invasion : invades muscularis propria (pT2)
7. Resection margin: free from carcinoma, safety margin: proximal 3.4 cm, distal 7.0 cm
8. Lymph node metastasis : no metastasis in 32 regional lymph nodes (pN0) (0/32: "1", 0/1; "3", 0/11; "4", 0/4; "5", 0/0; "6", 0/5; "7", 0/5; "9", 0/0; "8a", 0/1; "11p", 0/3; "12a", 0/2; "4sb", 0/0)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. AJCC stage by 8th edition: pT2 N0
註: EGC-like AGC로 부르는 것이 타당한 증례입니다.
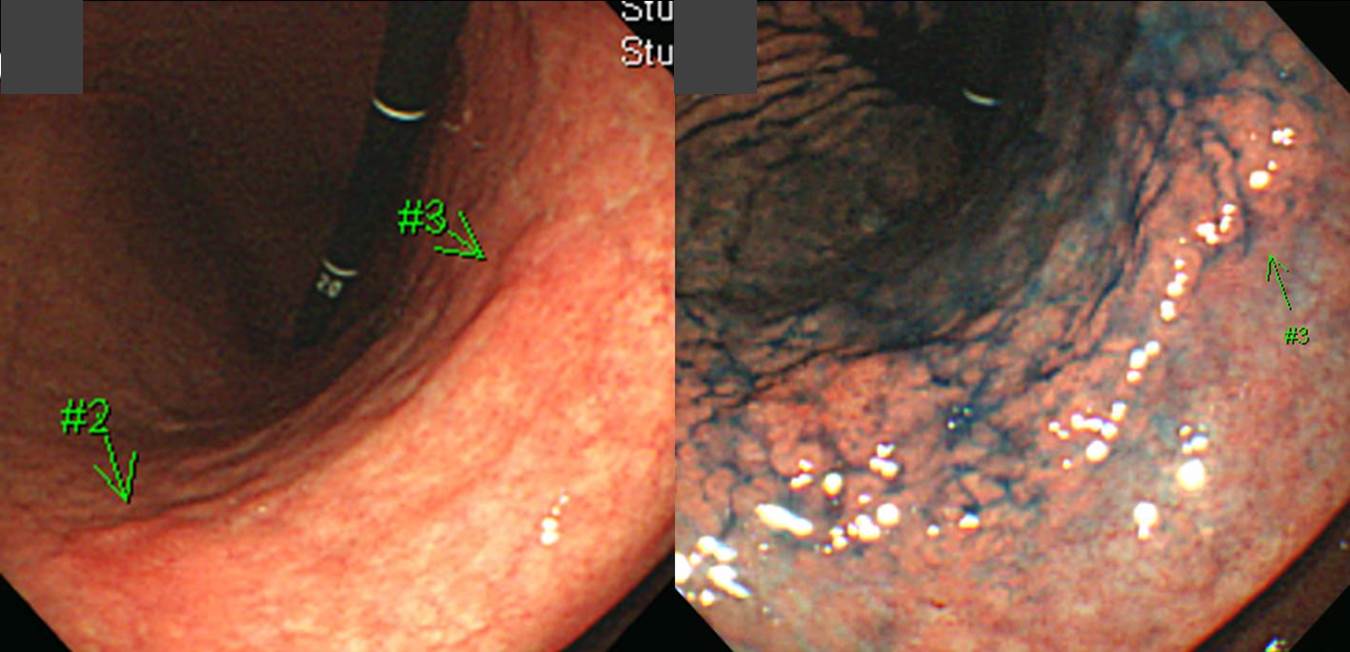
이 경우는 조직검사에서 moderatele differentiated로 나왔는데 병소의 경계가 매우 모호하였지만 여하튼 상당히 넓은 것으로 추정하였습니다. 수술 후 병리과에서도 크기를 다소 애매하게 써 주셨습니다.^^ 심달도는 SM3였고 림프절 전이는 없었습니다.

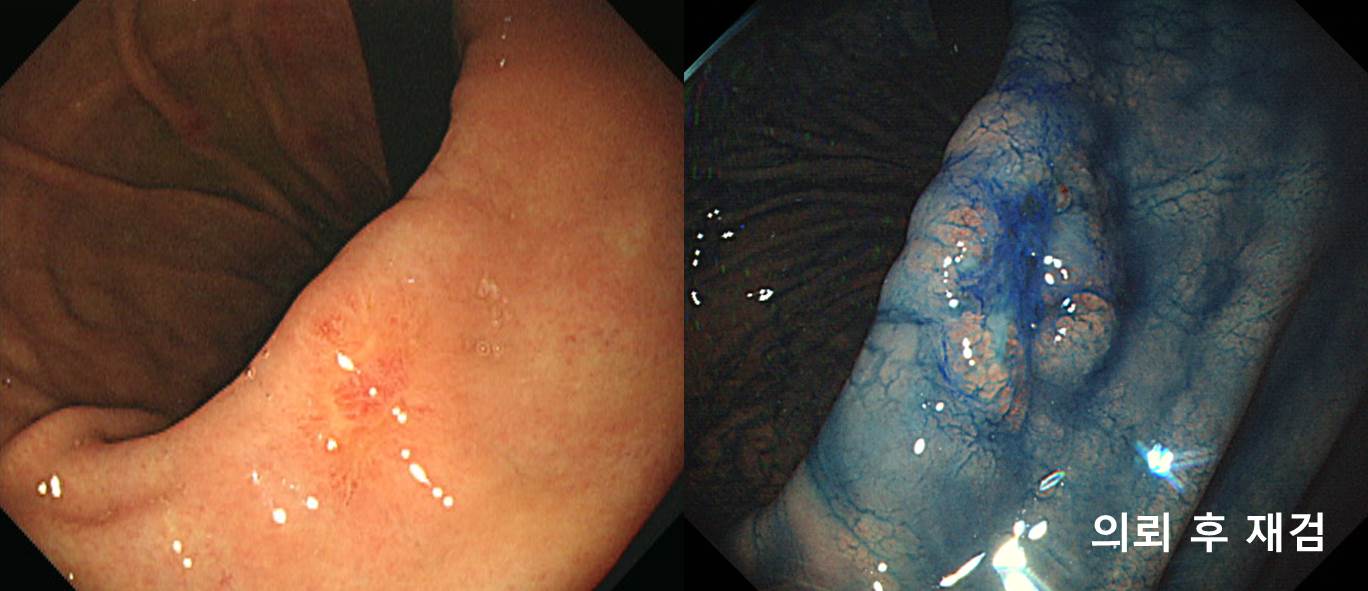
Stomach, radical subtotal gastrectomy: Early gastric carcinoma
1. Location : lower third, Center at antrum and circle
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size : encircling x 6.0 cm
6. Depth of invasion : invades submucosa (sm3) (pT1b)
7. Resection margin: free from carcinoma, safety margin: proximal 5.0 cm, distal 1.0 cm
8. Lymph node metastasis : no metastasis in 29 regional lymph nodes (pN0) (0/29 : "3,5", 0/9; "4,6", 0/8; "1", 0/1; "5", 0/1; "6", 0/4; "7", 0/2; "9", 0/1; "8a", 0/0; "11p", 0/2; "12a", 0/1; "4sb", 0/0)
9. Lymphatic invasion : present
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. Peritoneal cytology : negative
13. AJCC stage by 8th edition: pT1b N0
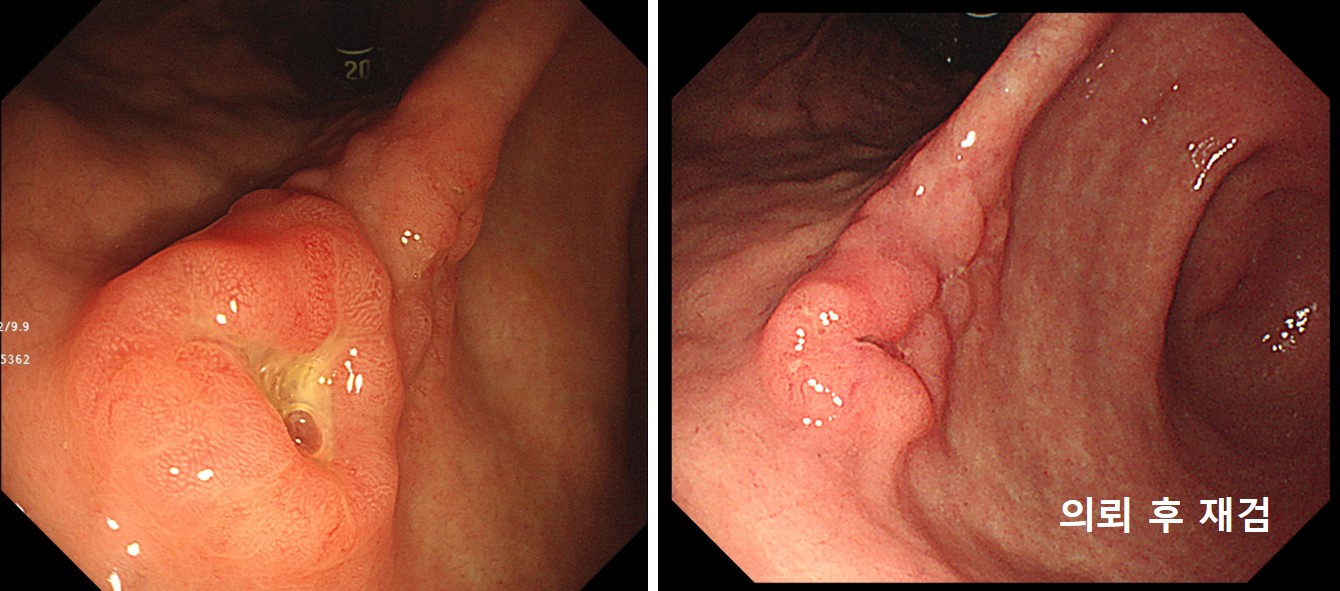
註: 첫 내시경 검사는 구형 Pentax 내시경이었고 의뢰 후 재검은 Olympus 260H 였습니다. 인간 위의 정상 색깔은 무엇일까요? 첫 내시경의 색조와 두번째 내시경의 색조 중간 어디가 가장 자연스러운 내시경 사진 아닐까 생각되었습니다. Pentax는 tone이 낮은 경향이 있어 검사가 차분하게 진행되지만 선명하지 않다고 이느끼시는 분들이 많습니다. Olympus는 tone이 높아 검사자를 흥분시키지만 선명하게 보인다고 느끼시는 분들이 많습니다. 사실 색조는 선명도와는 아무 상관이 없지만 느낌이 그렇다는 것입니다. 같은 모델이라도 색조가 조금씩 다르고, 오래 사용하면 색조가 다소 낮아지지만... 전체적인 진단율에는 별다는 영향을 주지 않는 것 같습니다. 취향과 습관 정도일 것 같습니다.
IIa+IIc 형 조기위암은 깊이가 점막하층인 경우가 많습니다. 그러나 모두 다 그런 것도 아니기 때문에 처음부터 수술을 권하기도 어렵습니다. EUS를 해도 별 도움이 안 되고......
ESD 후 수술
Early gastric carcinoma
1. Location : proximal antrum, postero-greater curvature
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 16 mm (2) vertical diameter, 14 mm
6. Depth of invasion : invades submucosa, (depth of sm invasion : 650 ㎛) (pT1b)
7. Resection margin : free from carcinoma(N), safety margin : distal 11 mm, proximal 12 mm, anterior 10 mm, posterior 12 mm, deep 200㎛ (sm only)
8. Lymphatic invasion : present (++)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
ESD 후 수술
Stomach, endoscopic submucosal dissection:
Early gastric carcinoma
1. Location : angle, lesser curvature
2. Gross type : EGC type IIa+IIc
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 16 mm (2) vertical diameter, 10 mm
6. Depth of invasion : invades submucosa, (depth of sm invasion : 1700 ㎛) (pT1b)
7. Resection margin : involved deep resection margin by carcinoma, safety margin : distal 13 mm, proximal 13 mm, anterior 8 mm, posterior 18 mm, deep 0 mm (sm only)
8. Lymphatic invasion : present (++)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
처음부터 수술
Stomach, radical subtotal gastrectomy: Early gastric carcinoma
1. Location : middle third, Center at body and lesser curvature
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, poorly (solid) differentiated
4. Histologic type by Lauren : diffuse
5. Size : 1.5x1.3 cm
6. Depth of invasion : invades submucosa (sm3) (pT1b)
7. Resection margin: free from carcinoma, safety margin: proximal 2.8 cm, distal 8.3 cm
8. Lymph node metastasis : no metastasis in 20 regional lymph nodes (pN0)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. AJCC stage by 8th edition: pT1b N0
전정부 소만 mid-antrum transverse fold에 위암이 놓여있으면 심달도 예측이 제법 어렵습니다. IIc라고 해야 할지 IIa+IIc라고 불러야 할지도 애매합니다. 저는 주변 융기부가 조금 현저하다고 보고 IIa+IIc에 준하여 판단하였습니다. 병리과에서는 IIc로 보았습니다. 내시경 치료 하기는 쉬운 위치이므로 조금 적극적으로 시도해 보기도 하는데, 이 환자에서는 함몰부위가 뚜렷하고 tumor island까지 있는 것이 영 마음에 걸려 바로 수술을 보냈습니다. SM3로 나왔습니다. 휴~~~
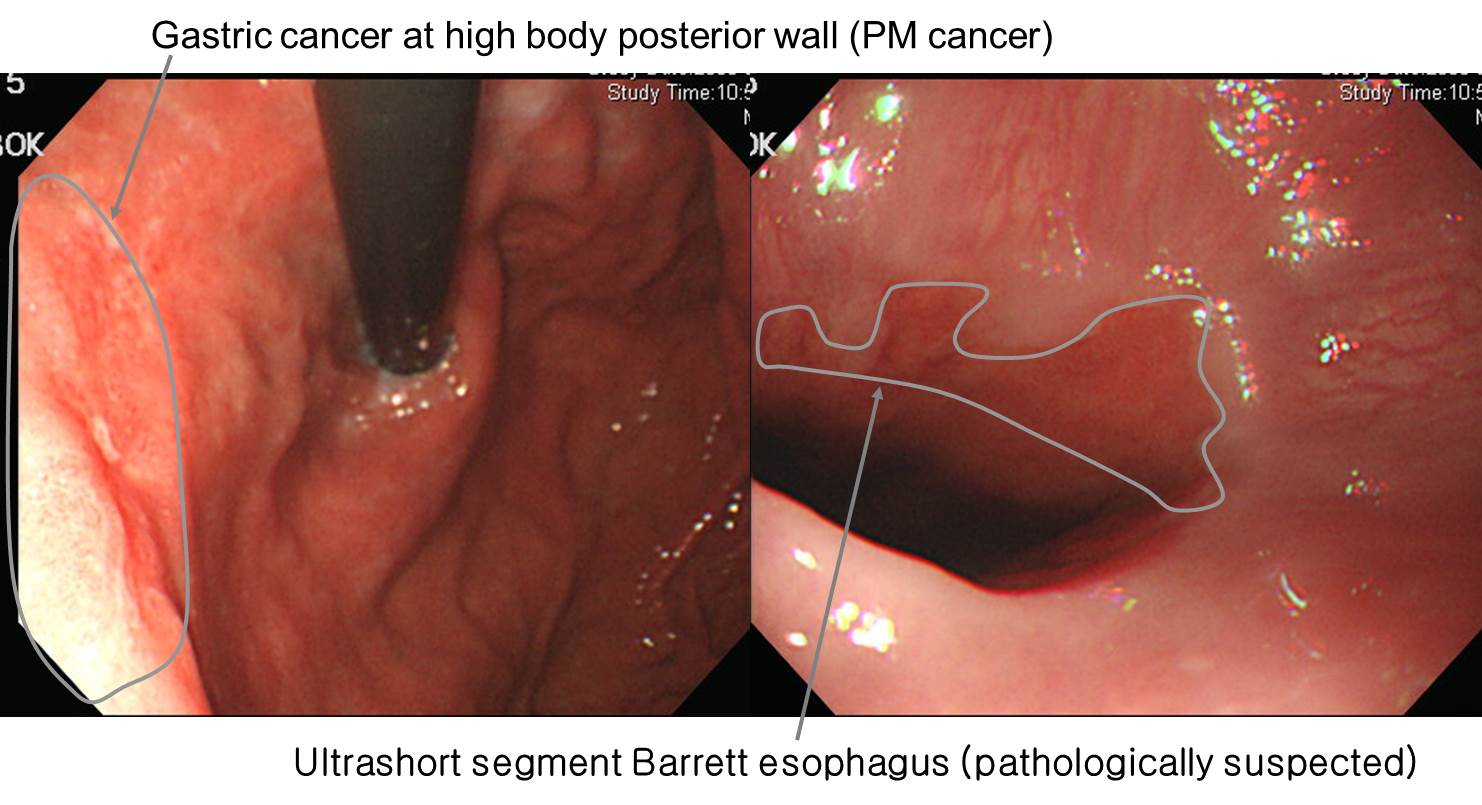
위체상부 후벽의 작은 depressed lesion이 발견되었고 내시경의는 당연히 EGC로 생각하였지만 병리결과가 의외로 아래와 같이 나왔습니다.Advanced gastric carcinoma
- Gross type : Borrmann type (unclassifiable) (mimicking EGC type IIc)
- Histologic type : tubular adenocarcinoma, poorly differentiated
- Size : 3.2x2.1x0.2 cm
- Depth of invasion : extension to proper muscle (pT2a)다시 봐도 역시 EGC라고 부를 수 밖에 없는 병소였습니다. 아무리 주의해도 EGC와 AGC를 나누는 정확도는 80-90%전후입니다. 물론 아주 definite한 EGC가 있고 반박할 수 없는 AGC도 있습니다. 그러나 많은 경우 우리의 예상이 틀립니다. 그다지 놀랄 일은 아닙니다.
이 환자에서 흥미로운 것은 병리과에서 Barrett esophagus가 있다고 연락을 해 준 점입니다. 사진을 review해보니 ultrashort segment Barrett esophagus가 있다고 말할 수 있는 그런 모양이었습니다. 그런데 곰곰히 생각해봅시다. 이 정도의 미세한 변화는 너무나 많지 않습니까? 오늘 내시경한 환자 중에도 이런 비슷한 모양을 보인 사람이 여러분 있었던 것 같지 않습니까? 이 환자의 경우에는 위암으로 인하여 수술을 하였기 때문에 하부식도의 조직의 양이 많아서 Barrett이라고 병리학적 진단을 할 수 있었던 예입니다. 그러나 forcep biopsy로는 어림 없지요. 대부분 진단되지 않습니다. 혹시 이런 짧은 바렛식도(저는 ultra ultra ultra-short Barrett esophagus라고 부릅니다)가 있는 경우 임상적 의의는 얼마나 될까요? 역시 1 cm이하의 매우 짧은 ESEM (endoscopically suspected esophageal metaplasia)는 우선 무시하는 것이 현실적일 것 같습니다. 1 cm이하의 ESEM에 관심을 가지느니 차라리 조기위암을 찾기 위하여 위를 좀 더 면밀히 관찰할 것을 권하고 싶습니다.
Stomach, subtotal gastrectomy:
Advanced gastric carcinoma
1. Location : lower third, Center at body and greater curvature
2. Gross type : Borrmann type 3
3. Histologic type : tubular adenocarcinoma, poorly (poorly cohesive) differentiated
4. Histologic type by Lauren : diffuse
5. Size : 3.7x1.4 cm
6. Depth of invasion : invades muscularis propria (pT2)
7. Resection margin: free from carcinoma, safety margin: proximal 2.3 cm, distal 9.4 cm
8. Lymph node metastasis : metastasis to 1 out of 37 regional lymph nodes (pN1), (perinodal extension: present) (1/37: "3", 1/11; "4", 0/11; "5", 0/0; "6", 0/0; "7", 0/4; "9", 0/0; "8a", 0/3; "11p", 0/2; "12a", 0/5; "4sb", 0/0; "1", 0/1)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : present
12. AJCC stage by 7th edition: pT2 N1이번 증례는 (1) 함몰부가 비교적 깊고, (2) fold fusion 소견이 여럿 관찰되고, (3) 조직형이 signet ring cell carcinoma이었으므로 눈으로 보기보다 다소 깊을 수 있을 여지가 많았던 경우입니다. 비록 내시경에서 EGC III (r/o submucosal cancer)라는 impression을 붙일 수 밖에 없지만... 약간 깊다고 나왔지만 놀랄 필요는 없을 것 같습니다.
Stomach, subtotal gastrectomy:
Advanced gastric carcinoma
1. Location : middle third, Center at body and greater curvature
2. Gross type : Borrmann type 3
3. Histologic type : tubular adenocarcinoma, poorly (poorly cohesive) differentiated
4. Histologic type by Lauren : diffuse
5. Size : 2.5x2.5 cm
6. Depth of invasion : penetrates subserosal connective tissue (pT3)
7. Resection margin: free from carcinoma, safety margin: proximal 3 cm, distal 11 cm
8. Lymph node metastasis : no metastasis in 70 regional lymph nodes (pN0), (0/70 : "3", 0/31; "4", 0/17; "5", 0/3; "6", 0/5; "7", 0/3; "9", 0/5; "8a", 0/4; "11p", 0/2; "12a", 0/0; "4sb", 0/0; "1", 0/0)
9. Lymphatic invasion : present (+++)
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. Peritoneal cytology : negative
13. AJCC stage by 7th edition: pT3 N0

Stomach, subtotal gastrectomy:
Advanced gastric carcinoma
1. Location : middle third, Center at body and greater curvature
2. Gross type : Borrmann type 2
3. Histologic type : tubular adenocarcinoma, poorly (poorly cohesive) differentiated
4. Histologic type by Lauren : diffuse
5. Size : 2.6x2.2 cm
6. Depth of invasion : invades muscularis propria (pT2)
7. Resection margin: free from carcinoma, safety margin: proximal 3.8 cm, distal 13.5 cm
8. Lymph node metastasis : no metastasis in 47 regional lymph nodes (pN0) (0/47: "3", 0/14; "4", 0/6; "5", 0/1; "6", 0/9; "7", 0/2; "9", 0/0; "8a", 0/2; "11p", 0/1; "12a", 0/2; "4sb", 0/10; "1", 0/0)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : present
12. Peritoneal cytology : negative
13. AJCC stage by 7th edition: pT2 N0
1. Location : middle third, center at body and posterior wall
2. Gross type : mimicking EGC type IIc
3. Histologic type : tubular adenocarcinoma, poorly differentiated
4. Histologic type by Lauren : diffuse
5. Size : 5x4x0.5 cm
6. Depth of invasion : extension to subserosa
7. Resection margin: free from carcinoma: safety margin
8. Lymph node metastasis : metastasis to 2 out of 35 regional lymph nodes (pN1)
9. Lymphatic invasion : present
10. Venous invasion : not identified
11. Perineural invasion : not identified
1. Location : middle third, center at body and lesser curvature
2. Gross type : Borrmann type (mimicking EGC type IIc+III)
3. Histologic type : signet-ring cell carcinoma
4. Histologic type by Lauren : diffuse
5. Size : 9.5x5.3x0.4 cm
6. Depth of invasion : extension to proper muscle (pT2a)
7. Resection margin: free from carcinoma: safety margin
8. Lymph node metastasis : metastasis to 9 out of 62 regional lymph nodes
9. Lymphatic invasion : present
10.Venous invasion : not identified
11.Perineural invasion : not identified
12.Associated findings : ulceration(ul IV)
Advanced gastric carcinoma
1. Location : lower third, Center at angle and lesser curvature
2. Gross type : Borrmann type 3
3. Histologic type : tubular adenocarcinoma, poorly (poorly cohesive) differentiated
4. Histologic type by Lauren : diffuse
5. Size : 2.4x2.2 cm
6. Depth of invasion : penetrates subserosal connective tissue (pT3)
7. Resection margin: free from carcinoma
8. Lymph node metastasis : no metastasis in 31 regional lymph nodes (pN0)
9. Lymphatic invasion : present
10. Venous invasion : not identified
11. Perineural invasion : not identified
Stomach, subtotal gastrectomy: Advanced gastric carcinoma
1. Location : middle third, Center at body and greater curvature
2. Gross type : Borrmann type 2
3. Histologic type : signet-ring cell carcinoma
4. Histologic type by Lauren : diffuse
5. Size : 3.6x2.7 cm
6. Depth of invasion : invades muscularis propria (pT2)
7. Resection margin: free from carcinoma
8. Lymph node metastasis : no metastasis in 44 regional lymph nodes (pN0)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : present
12. Peritoneal cytology : negative
13. AJCC stage by 7th edition: pT2 N0
EGC 아닌가 생각했는데 AGC였고 multiple lymph node 전이와 bilateral ovary metastasis까지 있었습니다.
(2012년, 50세 여성)
Stomach, radical subtotal gastrectomy: Advanced gastric carcinoma
1. Location : middle third, Center at angle and posterior wall
2. Gross type : Borrmann type 3
3. Histologic type : tubular adenocarcinoma, poorly (solid) differentiated >> mucinous adenocarcinoma (mucinous carcinoma portion: 20%)
4. Histologic type by Lauren : mixed
5. Size : 3.3x3.0 cm
6. Depth of invasion : penetrates subserosal connective tissue (pT3)
7. Resection margin: free from carcinoma, safety margin: proximal 3.3 cm, distal 3.8 cm
8. Lymph node metastasis : metastasis to 6 out of 32 regional lymph nodes (pN2) (perinodal extension: present) (6/32: "1", 0/2; "3", 2/2; "4", 2/9; "5", 0/0; "6", 2/5; "7", 0/4; "9", 0/6; "8a", 0/3; "11p", 0/1; "12a", 0/0; "4sb", 0/0)
9. Lymphatic invasion : present
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. AJCC stage by 8th edition: pT3 N2Ovary and salpinx, bilateral salpingo-oophorectomy : METASTATIC CARCINOMA, clinically from stomach
Location: Bilateral ovaries
Greatest dimension: 5.5 cm (left)
Lymphovascular invasion: PRESENT (focal)
Salpingeal extension: Absent (lymphovascular invasion only; left salpinx)
조직검사 M/D. ESD 아주 잠깐 고려하였다가 2cm가 넘고 경계가 불분명하여 수술을 보냈는데...
Stomach, radical total gastrectomy: Advanced gastric carcinoma
1. Location : upper third, Center at high body and lesser curvature
2. Gross type : Borrmann type unclassifiable (mimicking EGC type IIc)
3. Histologic type : tubular adenocarcinoma, poorly (poorly cohesive) differentiated
4. Histologic type by Lauren : diffuse
5. Size : 5.1x3.1 cm
6. Depth of invasion : invades serosa (pT4a)
7. Resection margin: free from carcinoma, safety margin: proximal 0.3 cm, distal 16.2 cm
8. Lymph node metastasis : no metastasis in 42 regional lymph nodes (pN0) (0/42: "1", 0/2; "2", 0/3; "5", 0/0; "6", 0/3; "7", 0/5; "9", 0/2; "8a", 0/2; "11p", 0/1; "12a", 0/1; "4sb", 0/0; "8p", 0/1; "lymph node", 0/1; 3,5, 0/9; 4,6, 0/12)
9. Lymphatic invasion : present
10. Venous invasion : not identified
11. Perineural invasion : present
12. AJCC stage by 8th edition: pT4a N0
W/D나 M/D와 같은 분화조직형 위암에서는 내시경 육안소견과 depth of invasion의 correlation이 비교적 좋습니다. 그러나, P/D나 SRC과 같은 미분화조직형 위암에서는 보기보다 깊은 경우가 많습니다.

Stomach, radical total gastrectomy: Advanced gastric carcinoma
1. Location : upper third, Center at body and posterior wall
2. Gross type : Borrmann type 3
3. Histologic type : tubular adenocarcinoma, poorly (poorly cohesive) differentiated
4. Histologic type by Lauren : diffuse
5. Size : 3.7x2.8 cm
6. Depth of invasion : penetrates subserosal connective tissue (pT3)
7. Resection margin: free from carcinoma, safety margin: p 2.7 cm, d 11.7 cm
8. Lymph node metastasis : metastasis to 3 out of 38 regional lymph nodes (pN2) (perinodal extension: present) (3/38: "2", 0/0; "3", 3/10; "4", 0/9; "5", 0/0; "6", 0/4; "7", 0/2; "9", 0/2; "8a", 0/5; "11p", 0/0; "12a", 0/2; "4sb", 0/0; "1", 0/4)
9. Lymphatic invasion : present(+++)
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. Peritoneal cytology : negative
13. AJCC stage by 7th edition: pT3 N2
[동영상] Depth of invasion of a small depressed lesion with focal wall thickening. 조기위암인가 진행성 위암인가?

2025-1-15. ECR
More cases
 6. 보만 1형 진행성 위암과 EGC type I의 구분
6. 보만 1형 진행성 위암과 EGC type I의 구분
보만 1형 진행성 위암과 EGC type I의 구분은 쉽지 않습니다. 가톨릭의대 김태호 선생님의 내시경학회 교육자료에서는 아래와 같은 언급이 있습니다.
Borrmann type I 형의 진행성위암과 EGCa I 형의 조기위암을 내시경 소견만으로 명확히 감별할 수는 없으나, 둔덕이나 bridging fold 와 같이 주변 점막의 변화, 겸자로 압박했을 때 밀리지 않는 소견은 점막하층 이상의 침윤이 있음을 시사하는 소견이다.
보만 1형 진행성위암이 커지면서 중앙에 함몰부가 발생하여 보만 2형이 되는 경우도 있을 것입니다. 경우에 따라서는 내시경의사는 보만 1형으로, 병리의사는 보만 2형으로 서로 다르게 분류하기도 합니다.
증례 사진(EndoTODAY 위암 481)을 보면 아시겠지만.... 엄밀한 의미의 보만 1형 진행성 위암은 흔하지 않습니다. 내시경에서 보만 1형 진행성 위암으로 추정하였어도 막상 SM cancer로 나오는 경우도 적지 않았습니다. 그러면... '환자에게는 다행스러운 일이군' 정도 생각하고 넘어갈 수 밖에 없을 것 같습니다. 요컨데 누구나 틀릴 수 밖에 없을 것 같으니 너무 신경쓰지 않으셔도 좋을 것 같습니다.
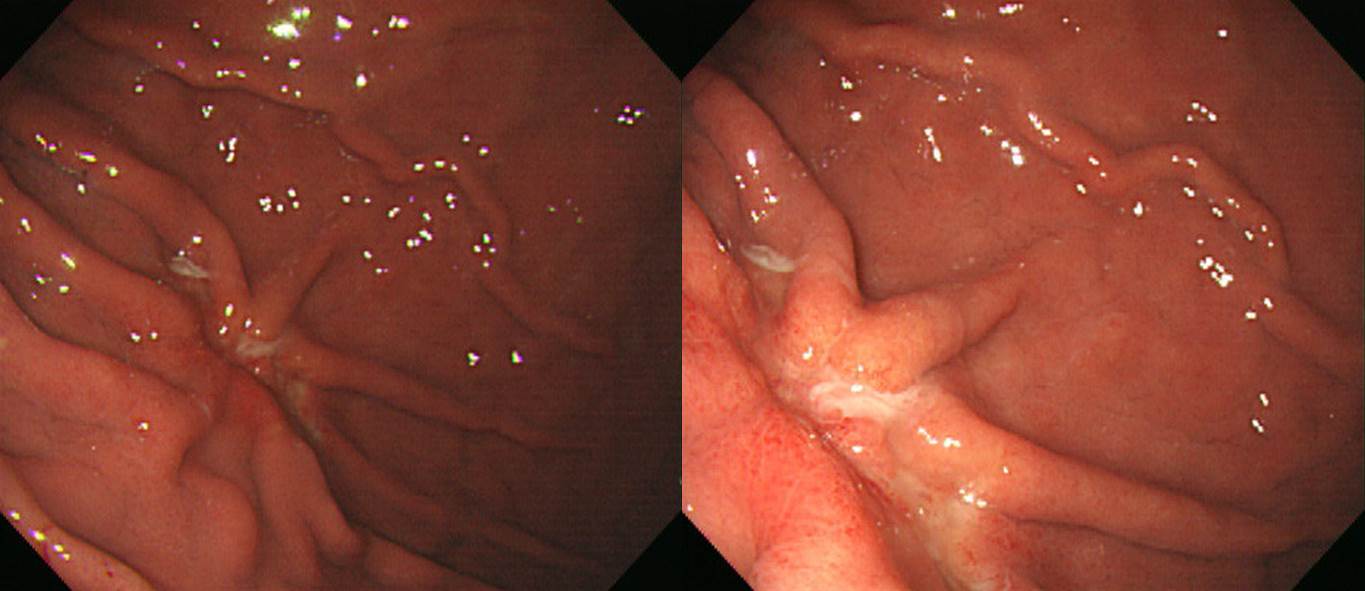
F/55. 다발성 위암. 위체하부 후벽에 함몰형 병소가 있고 근위전정부 후벽에 융기형 병소가 있다.
수술을 하였으며 함몰형 병소는 진행성 위암으로, 융기형 병소는 용종형 조기위암 (점막암)이었다.
암은 용종의 head에 국학되어 있었다. 일부 MM 층 아래의 종양이 보였으나 종양 주변으로 stroma가 함께 딸려오고 있으며 MM이 이 부위를 일부 감싸고 있어서 SM layer로 herniation된 점막암으로 해석하였다.
초심자는 이 병소를 AGC라고 불렀습니다. 전형적인 EGC인데...
STG: Early gastric carcinoma
1. Location : lower third, Center at antrum and lesser curvature
2. Gross type : EGC type IIa+IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size : 2.8x1.5 cm
6. Depth of invasion : invades mucosa (muscularis mucosae) (pT1a)
7. Resection margin: free from carcinoma. safety margin: proximal 12 cm, distal 1.7 cm
8. Lymph node metastasis : no metastasis in 16 regional lymph nodes (pN0)
9. Lymphatic invasion : not identified
10. Venous invasion : not identified
11. Perineural invasion : not identified
12. AJCC stage by 8th edition: pT1a N0
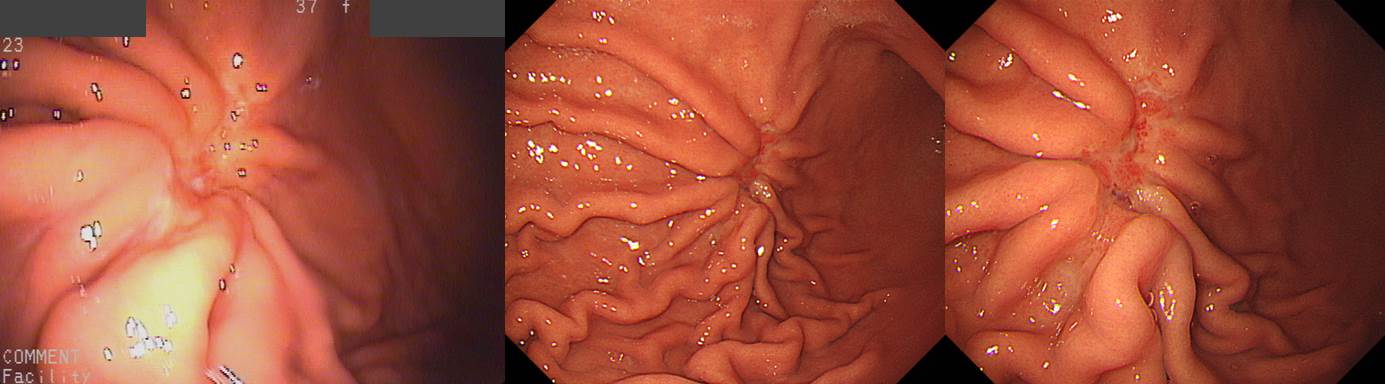
Fundus의 암은 생각보다 침윤이 깊을 수 있습니다. 이 증례의 depth of invasion을 어떻게 추측하십니까?
아래는 수술 결과입니다. 깊었고 림프절 전이도 심했습니다.
[2013-4-27. 애독자 편지]
침윤 깊이 (심달도) 진단"에 있어서 가장 중요한 것 중에 하나가 위병변의 위치라고 생각합니다. Antrum에 있는 II 병변들은 M > SM invasion일 가능성이 높지만, cardia에 있는 II 병변들은 SM > M invasion일 가능성이 높습니다. 따라서 흔히 우리가 알고 있는 "육안적 소견에 따른 침윤 깊이 (심달도) 진단"은 전정부에 있는 위암에서만 주로 적용이 되며, 위벽이 위로 갈수록 앏아지는 위체부 (특히 상방) 에서는 한 단계 더 깊은 침윤 깊이 (심달도)로 진단해야 한다는 것이 제 주장입니다.
[2015-1-29. 애독자 질문]
안녕하세요, 교수님. 최근 위암 증례에서 EGC-mimicking AGC, AGC-mimicking EGC 등에 대한 endotoday를 받아보면서 최근 내시경적 EGC/AGC 구분하는 방법이 뭘까 또한, 잘 구분하려면 어떻게 해야 하나 생각이 들었습니다. 외래에서 외부 병원 내시경 사진을 보고 AGC로 설명했는데, 본원에서 다시 내시경을 했더니 누가 봐도 EGC 였던 case를 경험하였습니다.
소화기내시경아틀라스에 적혀 있는 2910명의 분석과 91.3%의 구분에 대해서 논문을 찾아보니 반갑게도 삼성병원외과에서 썼지만, 선생님께서 함께 참여했던 논문이 있었습니다. (J Sur Onc, 2010;101:384-388) 2001~2003년까지의 2910명의 대규모 분석으로 좋은 기준(위치, 크기, 분화도, Lauren's type, ly+, v+, perineural invasion)을 알려주셨지만 자세히 읽어보니, method에서 EGC 진단과 AGC 진단에 차이를 두었습니다.
EGC : 바륨 또는 내시경상 EGC
AGC : 바륨과 내시경에서 모두 AGC이렇게 차이를 둬서, 실은 내시경 전문의를 지향하는 입장에서 barium study의 영향력을 구분하고 싶어졌습니다. 하지만 논문상에 내시경만으로 구분하는 입장을 보이는 연구는 거의 없고, 요즘은 NBI, EUS 등의 최신 기법에 대한 논문만 검색되었습니다. 다시 돌이켜서, 혹시 2910명 중, 내시경만 시행한 group에서의 차이는 어떻게 나왔는지 궁금해서 교수님께 이렇게 메일을 보냅니다. 아니면 이런 관련된 논문을 소장하시고 계신다면 알려주시면 감사하겠습니다.
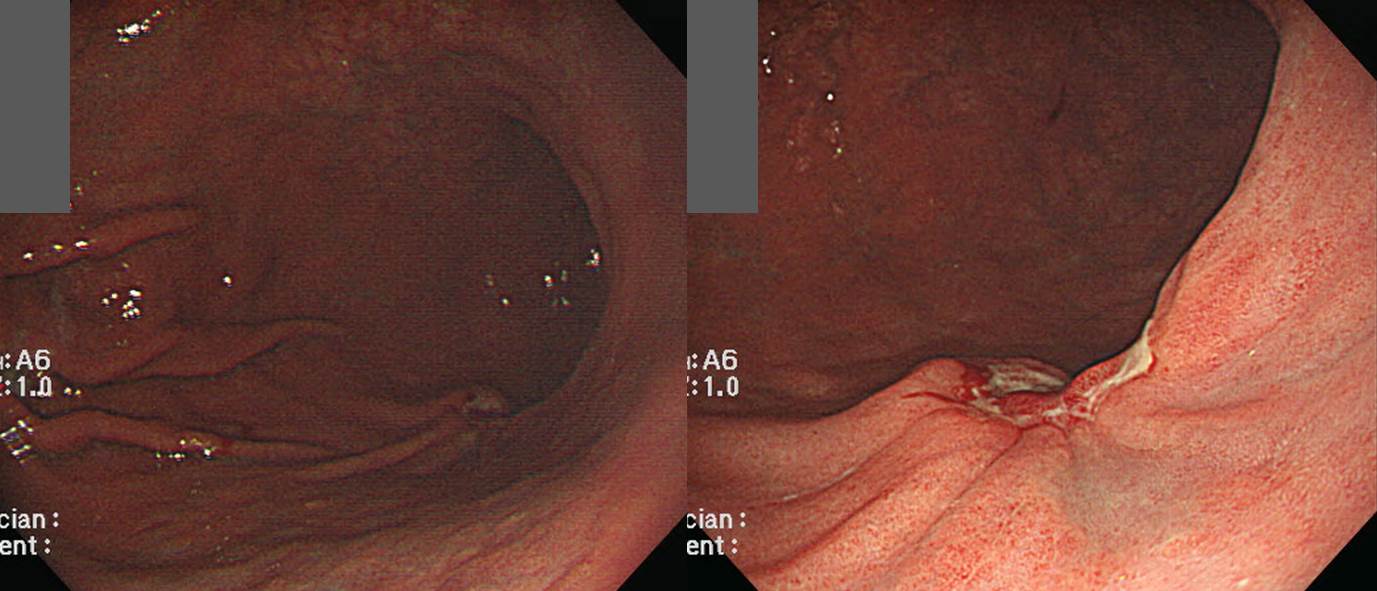
[조직검사에서 점막하침윤이 나온 증례, Submucosal invasion in forceps biopsy]
(1) 조직검사 점막하침윤. submucosal invasion in forceps biopsy (2) 점막하암에 대한 ESD. ESD for suspected submucosal cancer. 2025-9-22
1) 조기 위암에서 진행성 위암으로의 이행성 병변으로서의 고유근층 위암 김재규, 이준행 등. 대한소화기학회지 1999 (PDF)
2) [2013-4-17 대한소화기내시경학회 교육자료] 위암의 내시경 진단 분류 체계
3) Survey on endoscopic classification of EGC (EndoTODAY 2013-5-23)
4) 위암병리 가이드라인 (2023) - 우리말 version
5) AJCC 8th 해설 (김성은)
6) AJCC 8th PPT 인터넷 자료
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.