 EndoTODAY 내시경 교실
EndoTODAY 내시경 교실
Beginner | ESA | Schedule | OPD
Seminars | Atlas | Recent | Links
 [HNPCC. Hereditary nonpolyposis colorectal cancer] - 終
[HNPCC. Hereditary nonpolyposis colorectal cancer] - 終
2. Guidelines
3. 증례 모음
- 증례 1: 대장암, 위암, 소장암이 한 환자에서 발견
- 증례 2: HNPCC 환자에서 발견된 위암의 내시경 치료
- 증례 3: 대장암 가족력 많았던 HNPCC 환자의 소장암
- 증례 4: HNPCC 대장암으로 경과관찰 중 발견된 십이지장 암5. References
유럽소화기내시경학회에서는 HNPCC (Lynch syndrome)에 대한 가이드라인을 발표하였습니다 (Endoscopy 2019).
ESGE recommends that individuals with Lynch syndrome should be followed in dedicated units that practice monitoring of compliance and endoscopic performance measures. (Strong recommendation, low quality evidence, level of agreement 100%)
ESGE recommends starting colonoscopy surveillance at the age of 25 years for MLH1 and MSH2 mutation carriers and at the age of 35 years for MSH6 and PMS2 mutation carriers. (Strong recommendation, moderate quality evidence, level of agreement 100%)
ESGE recommends the routine use of high-definition endoscopy systems in individuals with Lynch syndrome. (Strong recommendation, high quality evidence, level of agreement 100%)
ESGE suggests the use of chromoendoscopy may be of benefit in individuals with Lynch syndrome undergoing colonoscopy; however routine use must be balanced against costs, training, and practical considerations. (Weak recommendation, moderate quality evidence, level of agreement 89%)
ESGE recommends definition of familial risk of colorectal cancer as the presence of at least two first-degree relatives with colorectal cancer or at least one first-degree relative with colorectal cancer before the age of 50 years. (Strong recommendation, moderate quality evidence, level of agreement 92%)
ESGE recommends colonoscopy surveillance in first-degree relatives of colorectal cancer patients in families that fulfill the definition of familial risk of colorectal cancer. (Strong recommendation, moderate quality evidence, level of agreement 100%)
대한장연구학회에서는 이번 가이드라인을 summary한 교육자료를 배포하였습니다. 감사합니다.
 3-1. 증례 1 - 대장암, 위암, 소장암이 한 환자에서 발견되었던 경우 (대장 증례 074)
3-1. 증례 1 - 대장암, 위암, 소장암이 한 환자에서 발견되었던 경우 (대장 증례 074)
대장암 가족력이 많은 (아버지, 어머니, 동생 등) 환자의 A colon 대장암이었습니다 (여성, 대장암 진단 당시 40대 초반). 질병의 이름에 non-polyposis가 붙어있지만 그래도 몇 개의 용종이 있는 경우가 많습니다. 이 환자에서도 대장암 이외에 6개의 용종이 있었습니다.

Ascending colon, cecum, appendix, and terminal ileum, right, hemicolectomy:
Adenocarcinoma, moderately differentiated, cecum:
1) tumor size: 5x3.5 cm
2) extension to the pericolic adipose tissue
3) endolymphatic tumor emboli: present
4) focal mucin production and micropapillary pattern
5) negative resection margins (proximal, 10 cm; distal, 13.7 cm)
6) metastasis to 1 out of 33 regional lymph nodes, (1/33: "right colic A", 0/1; "mid colic", 0/3; pericolic, 1/29)
. Multiple tubular adenomas, high-grade dysplasia (x6)
. Appendix with no diagnostic abnormalities recognized
AJCC Pathologic Stage IIIB (T3, N1, MX)
유전자 검사에서 MSI-H (BAT 25: unstable, BAT 26: unstable, D5S346: unstable, D17S250: stable, D2S123: unstable)가 나왔고 MLH1 유전자의 frameshift mutation이 확인되었습니다.
대장암 수술 10년 후 위암도 발견되어 ESD를 하였습니다.
Stomach, endoscopic submucosal dissection:
Early gastric carcinoma
1. Location :angle
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, well differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 16mm (2) vertical diameter,11 mm
6. Depth of invasion : invades mucosa (lamina propria) (pT1a)
7. Resection margin : free from carcinoma(N), safety margin : distal 11 mm, proximal 10 mm, anterior 16 mm, posterior 22 mm
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
위암 수술 2년 후 십이지장의 SMT-like cancer가 발견되어 수술을 하였습니다.

Duodenal Carcinoma
(1) Histologic type: Signet ring cell carcinoma with mucin production (60%)
(2) Histologic Grade: G3 (poorly differentiated)
(3) Precursor lesion: not applicable
(4) Invasive tumor size: greatest dimension (3cm)
(5) T4: Tumor directly invades pancreas and periduodenal soft tissue
(6) N1: Metastasis 2 out of 7 regional lymph nodes, (2/7: LN8, 0/1; LN12, 0/4; periduodenal, 2/2)
(7) cM0: Clinically No distant metastasis
(8) Involvement of portal vein: absent
(9) Margin status: Duodenal margin: negative (safety margin: 3 cm); Pancreas neck margin: negative
(10) Perineural and neural invasion: present
(11) Lymphovascular invasion: present
(12) Autolysis, gallbladder
[해설] HNPCC-associated cancer에는 대장암 이외에 자궁내막암 (lifetime risk 54%), 난소암 (lifetime risk 10-12%), 위암 (lifetime risk 13% or higher in Korea), 간담도암, 소장암, 신장암 등이 있습니다.
 3-2. Case 2: HNPCC 환자에서 발견된 위암의 내시경 치료
3-2. Case 2: HNPCC 환자에서 발견된 위암의 내시경 치료
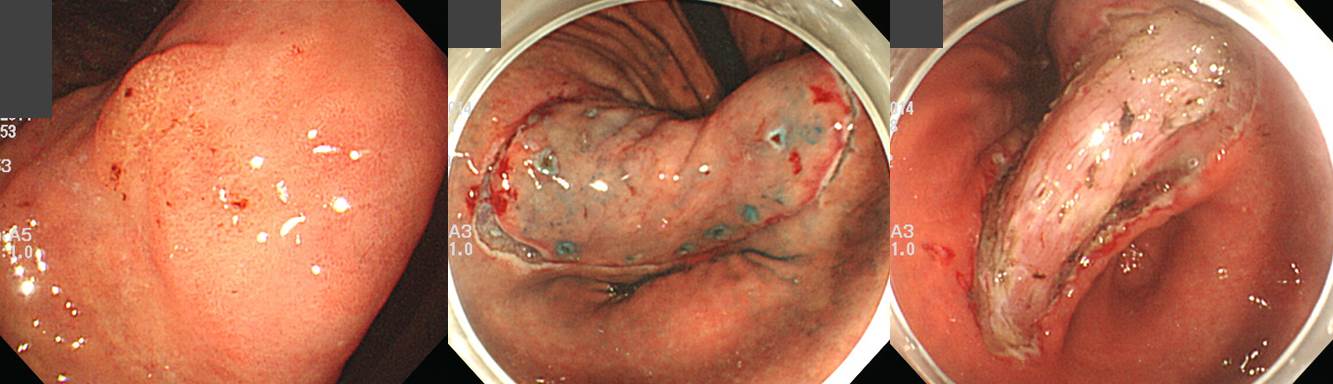
10여년 전 대장암으로 수술을 받으신 HNPCC 환자가 위암이 발견되어 의뢰되었습니다. 일반적인 ESD 적응증에 해당하여 시술을 하였고 아래와 같은 결과였습니다.
ESD: Early gastric carcinoma ;
1. Location : angle, posterior wall
2. Gross type : EGC type IIc
3. Histologic type : tubular adenocarcinoma, moderately differentiated
4. Histologic type by Lauren : intestinal
5. Size of carcinoma : (1) longest diameter, 18 mm (2) vertical diameter, 12 mm
6. Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
7. Resection margin : free from carcinoma(N), safety margin : distal 12 mm, proximal 11 mm, anterior 14 mm, posterior 12 mm, deep 600 ㎛
8. Lymphatic invasion : not identified(N)
9. Venous invasion : not identified(N)
10. Perineural invasion : not identified(N)
11. Microscopic ulcer : absent
12. Histologic heterogeneity: absent
일반적인 HNPCC surveillance를 하시도록 권하였고, 위암 ESD 후 추적관찰은 다른 환자와 비슷하게 하려고 합니다.
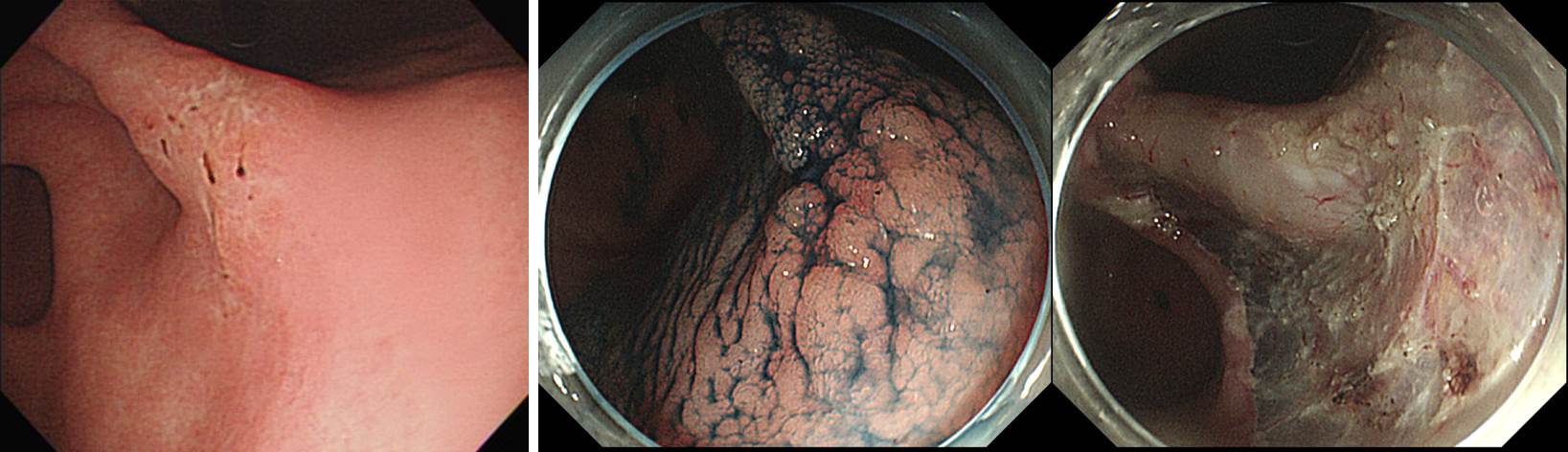
 3-3. Case 03: 대장암 가족력 많았던 HNPCC 환자의 소장암
3-3. Case 03: 대장암 가족력 많았던 HNPCC 환자의 소장암
Small bowel enteroscopy 소견
Small intestine, segmental resection: Adenocarcinoma, moderately differentiated, jejunum:
1) tumor size: 6x3.5 cm
2) tumor invades subserosa (T3)
3) lymphovascular invasion: not identified
4) perineural invasion: not identified
5) negative resection margins
6) no metastasis in 15 regional lymph nodes (0/15: "lymph node", 0/14; peri-jejunal, 0/1)
<< Result of immunohistochemistry >>
MLH1: Stained in about 95 % of tumor cells
MSH2, MSH6: Stained in 0 % of tumor cells
p53: Stained in about 1-5 % of tumor cells
<< Addendum (M11-14973)>> Multiplex PCR and Analysis with 3130xl Genetic analyzer
NR27, NR21, BAT26, BAT25, NR24 : all unstable
 3-4. Case 4: HNPCC 대장암으로 경과관찰 중 발견된 십이지장 암.
3-4. Case 4: HNPCC 대장암으로 경과관찰 중 발견된 십이지장 암.
HNPCC에서는 대장암 이외의 다른 많은 장기의 암이 발견될 수 있습니다. 소장암도 적지 않은데요... 소장암 중에서는 duodenal cancer가 가장 흔합니다. 이 환자에서는 1부와 2부 경계인 SDA (superior duodenal angle) 에서 암이 발생하였습니다만, 이보다 distal에서도 발생할 수 있습니다. Screening endoscopy에서 가능하면 십이지장을 깊게 관찰하시기 바랍니다.
HNPCC에서는 정말 검사할 부위가 많습니다. 환자들이 참 힘들 것 같습니다.
1) 폴립증후군 - 내시경세미나 강의록. 서울대학교 임종필. PDF 0.7M
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.