 [Duodenal varix. 십이지장 정맥류]
[Duodenal varix. 십이지장 정맥류]
Previous | Home | EndoTODAY | List | Next
십이지장 정맥류는 간과되기 쉽습니다. 조직검사 후 출혈이 발생할 수 있습니다. 정맥류의 가능성이 있다고 판단되면 절대로 조직검사를 하지 마십시오.
십이지장 정맥류에서 조직검사 후 출혈한 경우인데 다행스럽게 곧 멎었습니다.
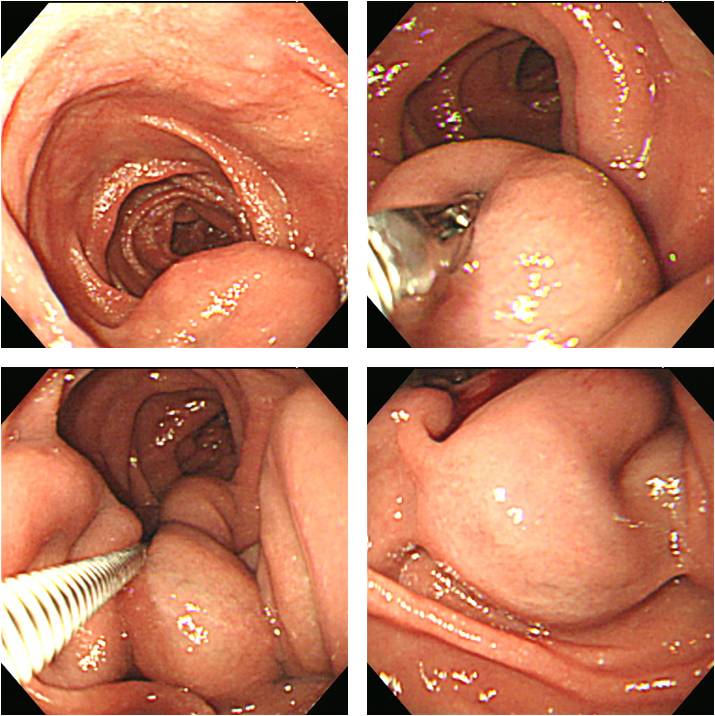
Budd chiari syndrome 환자에서 발견된 십이지장 정맥류입니다.
간암 환자의 반복적인 십이지장 정맥류 출혈로 clipping와 histoacryl로 지혈술을 하였으나 출혈이 반복되었던 환자입니다. (F/60, 2017)
Fatal duodenal varix bleeding
[문헌 증례]
A 30-year-old man with a history of alcoholic cirrhosis presented with 1 week of melena and 1 day of lightheadedness. On initial presentation, the patient was tachycardic (heart rate 123 bpm); blood pressure was normal. Physical exam was remarkable for mild abdominal distension. In laboratory tests at admission, hemoglobin concentration was 5.2 g/dl, platelet count was 141, 000/μl, and international normalized ratio was 1.3. Total bilirubin was slightly elevated: 1.5 mg/dl. The results of other liver-function tests were within normal limits. Esophagogastroduodenoscopy showed a large (>5 mm) varix with a nipple sign (a) in the second portion of the duodenum. Computed tomography of the abdomen showed stigmata of portal hypertension, including paraduodenal varices (b). Portal venography demonstrated dominant duodenal varices originating from the superior mesenteric vein and inferior vena cava. Portosystemic gradient was measured at 6 mm Hg. Coil embolization of the duodenal varices was successful (c). Bleeding from duodenal varices is rare but potentially fatal; the nipple sign on a varix correlates positively with recent severe bleeding and warrants urgent intervention. (Am J Gastroenterol 2017)
A 78-year-old woman presented with 500 mL hematochezia, hypotension, and a hemoglobin level of 5.4 g/dL. She had a history of right hemilobectomy of the liver and hepatojejunostomy for Klatskin tumor IIIA at other institutions 2 years before. Her medical history also included mitral regurgitation. Emergency esophagogastroduodenoscopy revealed a large, bluish, rugged mass with a smooth surface in the 3rd portion of the duodenum. A red spot was observed at the middle of the lesion (Fig. A). Contrast-enhanced CT of the abdomen revealed a brightly enhanced mass without lobulation in the same location (Fig. B, arrow). What was her diagnosis, and how would you treat the patient? Her diagnosis was duodenal varices. First, endoscopic band ligation of the varices was considered. However, the lesion was too huge to be obliterated completely. Endoscopic sclerotherapy could not be performed because of the risk of lipiodol embolization through a large-bore efferent systemic shunt from the varices. Therefore, the patient underwent angiographic embolization under fluoroscopic guidance, and the lesion was successfully obliterated. Three days after vascular intervention, follow-up endoscopy revealed slight discoloration and reduction of the varices without evidence of bleeding (Fig. C). Further regression of the varix was observed on follow-up endoscopy after 1 week (Fig. D). Finally, the duodenal varix completely disappeared 3 months after the intervention (Fig. E). (Intest Res 2017)
[Brief review]
부산대학교 김광하 교수님께서 대한임상소화기내과에 기고하신 글 중 십이지장 정맥류에 해당하는 부분을 옮깁니다.
경상대학에서 대한소화기내시경학회지(2008;36:292-297)에 기고한 글의 일부를 옮깁니다.
"간문맥 고혈압 환자에서 발생하는 정맥류 출혈은 대량 출혈 및 재출혈 빈도가 높아서 빠르고 정확한 진단과 치료가 요구되는 응급질환이다. 출혈 부위는 식도 및위 정맥류 출혈이 대부분이지만 드물게는 이소성으로 십이지장, 공장, 회장, 충수돌기, 하행결장, 직장 및 S자결장 등에서도 발생할 수 있다. 그 중 십이지장 정맥류는 이소성 정맥류의 1/3을 차지하고 출혈은 거의 발생하지 않는 것으로 알려져 왔다. 그러나 일단 출혈하게되면 생명의 위협이 될 정도로 심하다. 최근에는 십이지장 정맥류 출혈 시 비수술적인 방법으로 내시경적 경화 술, 내시경적 결찰술, 경정맥 간내문맥-간정맥 단락술(transjugular intrahepatic portosystemic shunt) 등이 보고되고 있지만 아직 효율적인 치료방법은 정립되어 있지 않다."
Ginsberg textbook 2005에서 옮깁니다.
In portal hypertension, varices can also develop in other parts of the GI tract including the anorectal region, colon, and small intestine. Portal hypertensive gastropathy, colopathy, and enteropathy are other sequelae. Primay duodenal varices are rare and are usually found incidentally at the time of endoscopy, more often in patients with extrahepatic portal vein obstruction or in cirrhotics with portal vein thrombosis. Usually the afferent vessel of the duodenal varices is the superior or inferior pancreaticoduodenal vein originating in the portal vein trunk or superior mesenteric vein. The efferent vain drains into the inferior vena cava. In a review of 169 cases of bleeding ectopic varices, 17% occurred in the duodenum, 17% in the jejunum or ileum, 14% in the colon, 8% in the rectum, and 9% in the peritoneum.
© 일원내시경교실 바른내시경연구소 이준행. EndoTODAY Endoscopy Learning Center. Lee Jun Haeng.